INTRODUCTION
Massive bone loss of the proximal femur recognizes various etiologies: post-traumatic, oncological, periprosthetic fractures, aseptic and septic loosening for periprosthetic joint infections.1–3 The current definition of major proximal femur defect (MPFD) is identified by the Paprosky classification type IIIB (less than 4 cm of diaphyseal bone available) and IV (widened diaphyseal bone available).4 The management of an MPFD still remains controversial and challenging. Nowadays there are several surgical treatment options available: reconstruction with extensively porous coated stem,5 bone grafting,6 modular and monoblock cementless stems,7 allograft prosthetic composite,1 proximal femoral replacement,8 and resection arthroplasty and reconstruction by modular mega-prosthesis.9
Parameters such as etiology, age, comorbidities, previous walking ability and will of the patient were taken into consideration. The concept of the mega-protheses (MP) was first defined a few decades ago to manage skeletal reconstructions after extensive tumor resections.10 Over the years, the old monolithic implants have been replaced by modular implants which brought versatility to the system and greatly promoted the surgical technique.11,12 The application field of mega-prostheses has therefore been expanded to other sectors of orthopedics and trauma surgery.
Proximal femur reconstruction with mega-prostheses is believed to be technically less demanding than other complex reconstructive procedures due to extensive bone loss, including allograft prosthetic composite (APC). The surgery is usually shorter and allows a relatively early rehabilitation. However, this type of implant has disadvantages among which an increased risk of dislocation, due to the loss of functioning and infection.12
The purpose of the study is to present our experience with the use of proximal femur mega-prosthesis in MPFD.
MATERIALS AND METHODS
From 2006 and 2018, forty-four patients suffering from major proximal femoral defects, underwent implantation of proximal femur mega-prosthesis. Inclusion criteria were: major proximal femoral defects due to periprosthetic fractures, previous arthroplasty infection (second stage of a two stage strategy), implant failure, aseptic loosening. Exclusion criteria were: oncological patients, active infections, follow-up less than 1-year.
Surgical technique and surgical access varied according to the etiopathogenesis. All procedures were performed by the same senior surgeon.
Revision hip surgical technique for periprosthetic fractures
The surgical technique of choice consisted in a lateral access at the hip with the patient in supine decubitus. The old prosthetic implant was removed, ensuring the preservation of a good quality of residual bone in order to fix it to the new implant. A large resection modular stem (GMRS, STRYKER, Mahwah NJ) was cemented into the residual femoral canal. In five cases the acetabulum was implanted because it appeared loosened. Hemispherical acetabular cup was applied, with morselized bone chips to fill the defects.
Revision hip surgical technique for periprosthetic osteolysis
A direct lateral access to the patient’s hip in supine decubitus was performed in nine cases, and a modified Smith Petersen Wagner access was performed in six cases. The type of access was established evaluating the acetabular bone loss and the severe “up and pelvic discontinuity” defects. On the femoral side, once the implant was removed and the inadequate support of the metaphyseal and isthmic area was ascertained, the implantation of the cemented MP was performed after appropriate trials. The good quality residual bone was repaired on the implant with metal rims.
Surgical Technique for Revision Implant Failures for Recalcitrant Infections
In supine decubitus, Wagner modified Smith Petersen access was performed in all cases. All patients in the series had previously undergone hip excision arthroplasty for recalcitrant infections. Once the acetabulum was made prosthetic, the femur was approached with the implantation of a cemented mega-prosthesis in the residual canal, after appropriate trials.
After implantation of megaprosthesis the muscle and ligament were re-inserted on prosthesis through appropriate holes on MP. One sub-fascial vacuums drainage was positioned and then removed after 48 hours.
All patients received one-shot antimicrobical therapy thirty minutes before the surgery based on epidemiological analysis of local bacterial species. All patients wore antithrombotic stockings and taken low-molecular-weight heparin until full weight bearing was achieved.
In all the operated cases, the rehabilitation protocol was mostly dependent on the acetabulum component: early loading on the third day in cases of non-revised acetabulum and in Paprosky type I-II acetabular revisions. Loading was instead postponed for several weeks in Paprosky type 3A-3B acetabular revisions and in cases of pelvic discontinuity according to radiographic follow-up. Monthly for first six months, then every six months, all patients performed a clinical and radiographical examinations. During outpatients visit, in the final follow-up, Merle D’Aubignè and Postel hip rating scale was submitted: the score includes evaluation of pain, ability to walk and range of motion on a scale from a minimum of 1 point (worse score) to 6 points (better score). Osteointegration and radiolucent lines were evaluated by radiographic examinations. Osteolysis was defined as the appearance of a radiolucid zone in the pelvic area around the acetabulum and in the femoral shaft near the femoral stem.13
During the hospitalization and outpatient follow-up all the complications were recorded (wound dehiscence, deep infection, pneumonia and urinary tract infection). Wound dehiscence or surgical site infection was defined as a delayed of normal healing of the surgical wound with presence of redness, edema and secretion in absence of deep tissue involvement or general symptoms.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Local Ethical Committee. The authors declare no conflict of interest. Informed consent was obtained from all individual participants included in the study.
RESULTS
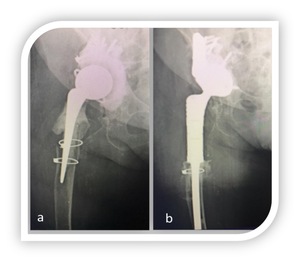
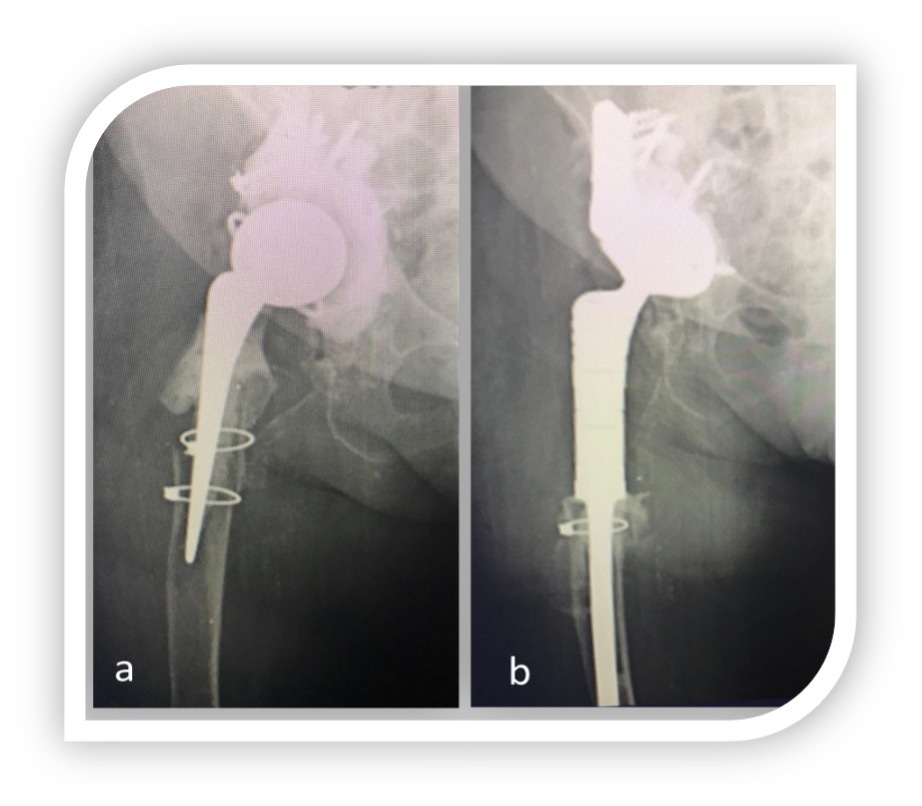
Forty-four patients were included in the study. At 5 years follow-up (2.1 to 6.5), 39 patients, 23 female and 16 males, were alive. Four patients died for non-related surgery causes; one was lost at follow up. The etiopathogenesis was represented by periprosthetic fractures (6), periprosthetic osteolysis (15), revision implant failures for recalcitrant infections (18).(Fig 1, 2) The average age was 69 years (47 to 78).
According to the Merle D’Aubignè and Pastel card (pain, mobility and walking ability) no patient exceeded 10 points. In particular the periprosthetic fractures had an average score of 9.2 points, the periprosthetic osteolysis showed 6.7 points, and recalcitrant infections 6.2 points. The best results were observed in patients with periprosthetic fractures. No patient in the two series exceeded nine points on the Merle D’Aubignè and Pastel hip rating scale.
All complications occurred during the first-year follow-up. We recorded eight complication (8/39 patients, 20%): one transient paralysis of the external popliteal nerve, during perioperative time, resolved at the end of the third month; three surgical site infections managed with debridement, washing of the wound and antimicrobial therapy; two dislocation and two periprosthetic fracture and dislocation, in these cases acetabular component was revised with a retentive cup (constrained liners).
Regarding limb length: ten patients had no residual dysmetria, two had a residual dysmetria of about one centimeter, seven had a dysmetria between one and two centimeters. At last follow-up all patients used two sticks.
At last follow-up all implants were osteointegrated even in presence of thin striae of femoral radiolucency in most reported cases. In particular 16 radiolucency were noticed (3 in periprosthetic fractures, 7 in periprosthetic osteolysis and 6 in recalcitrant infections). No patients showed clinical symptoms related to radiolucency.
DISCUSSION
There is relatively little published literature regarding the use of mega-prostheses in non-oncologic patients and all are retrospective case series.1,2 The mega-implants were originally born to meet the needs in cancer surgery after extensive resections of bone segments for primary or repetitive injuries.14,15 Over the years, the large resection prosthesis has been used both in trauma surgery, for complex fractures and periarticular pseudarthrosis, and in revision surgery.2,16,17 Failed hip arthroplasty with extensive bone loss (due to infection, fracture or aseptic loosening) was the most common non-neoplastic indication for proximal femur megaprosthesis.18
The modern modular mega-implants that replaced monoliths, while making the surgical technique simpler and more versatile. Limb dysmetria, infections, instability, femoral radiolucency, limp leg are common complications.14,19
In our series we observed lower complication rates respect to the recent literature; seven patients were surgically (18%) treated within five years. Similar results concerning the reoperation rates were reported by Viste et al (18%),20 but lower values were reported by Grammatopulos et al which analyzed 79 PFRs for non-neoplastic conditions at 5 years, showing a complication rate of 22% and a revision surgery rate of 11%.21 However, higher complication rates were reported by Korim et al (24%),22 Fenelon C et al (22,8%) and De Martino et al (22%) with a recent retrospective review of 41 PFR treated in a single institution, using the same revision stem.11,23
Dislocation was the most common complication with a multifactorial etiology. The most important causes of instability included: the inability to achieve a standard repair of the residual soft-tissue due to multiple previous procedures, the compromise of the abductor mechanism and the comorbidities of the elderlies.14,15,24 Our dislocation rates were relatively comparable (10%) with those reported by Viste et al (14%),20 Vaishya et al (14,6%) and Korim et al (16%).18,22 On the other hand we noticed higher dislocation rates than De Martino et al (5%)11 and Grammatopoulos et al (3,7%) probably because we didn’t use routinely constrained liners, which were reserved only for recurrent dislocations, as last resource.21
Soft-tissue complications in our cohort included 3 infections of the wound (8%) managed with surgical debridement and antibiotic therapy and 1 neurologic complication (3%) reported with a transient paralysis of the external popliteal nerve resolved spontaneously. Our data were comparable with Korim et al (reoperation rate ranged from 13,3-40%), a recent meta-analysis of 14 studies including a total of 356 RTHA surgically treated with MP,22 Henderson et al (5,2%),25 which reported a lower rate of soft-tissue complications including disclocations, while instead Vaishya et al showed the lowest rates (1,2%).18 All implants in our series were osteointegrated even in the presence of thin femoral radiolucency striae present in most reported cases. All patients used sticks for a clear limp leg.
In our series we reported the worst results of leg-length discrepancy in cases with periprosthetic osteolysis and recalcitrant infections. Despite ten of 39 patients had no dysmetria, we observed a dysmetria of about 1 cm in twenty-two patients (56%) and 1-2 cm in five patients (13%). A large number of articles have analyzed the functional outcomes of the patients undergoing mega-prosthesis for proximal femur bone loss while Al Taki et al evaluated the degree of improvement in pain, in function and in global quality of life measured by validated scores.26,27 Their data reported an important improvement in the quality of life comparable to the result obtained after RTHA using a conventional hip revision system. Our data examined the functional outcomes with Merle D’Aubignè and Pastel scale observing a higher score in patients undergoing proximal femoral replacement for severe bone loss with previous periprosthetic. According to Fenelon et al it is essential in this type of patients with poor proximal femoral bone stock and a prolonged restricted weight-bearing period to provide a stable platform to walk on.23 The authors believed that the most important factors that determine the overcoming of the PFR were the immediate unrestricted weight-bearing with aggressive physical rehabilitation. In fact, a stable and quickly cemented fixation with MP is a low demanding technique in elderly, osteoporotic, low-demand or sedentary patients which allowed a rapid mobilization for the prevention of prolonged bed rest syndrome.28 Other studies reported good hip outcome scores after PFR in patients with periprosthetic fractures.29
Sculco et al authored a review on the management of the femoral bone loss in revision total hip arthroplasty where it was stated that the role of proximal femoral megaprosthesis should be considered only as salvage solutions, particularly in the treatment of elderly, low-demand or sedentary patients.30
Megaprosthesis represent a rescue surgery for selected patients as oncologic and complex elderly. We are of the opinion that a better reattachment system of the abductor mechanism to the prosthesis, appropriate dual mobility cup or constrained liners and rigorous cementation are all elements that can reduce the complication rates and speed up the functional recovery.
This study has several limitations. The size of the study is small, because those procedures are rare. Furthermore, it is a retrospective series with all the biases of retrospective studies. The etiology of patients were disomogenous and there are several missing data (comorbidity of the patients, anthropometrics data, surgery related factor, no preo-operative functional scores). However, we collected one of the largest contemporary series present in literature.
CONCLUSION
Patient with severe proximal femoral bone loss is a real challenge also for expert surgeons. These patients, especially who previously presented septic should be considered like oncologic patients and treated by an aggressive surgery to allow an immediate weight bearing and fast rehabilitation. Mega-prosthesis should be considered as an effective opportunity to restore function and quality of life in patient with highly crippling disease.