INTRODUCTION
The treatment of complex acetabular fractures (T-shaped, both columns, transverse, anterior and hemi-transverse posterior, transitional form) represents one of the most challenging procedures performed by orthopedic surgeon. Anatomical reduction of fractures is the base of treatment, due to unsatisfied results following conservative management.1,2 It is well known that an easy access to the fracture site and good visualization of the surrounding structures are required to perform an anatomic reduction. Several surgical approaches have been proposed. Anterior (ilioinguinal) and posterior (Kocher-Langenbeck) approaches represent the most common.3 In the last years, the anterior intrapelvic approach, known as modified Stoppa approach has been widely spread.4 It provides access to the medial wall of acetabulum, quadrilateral surface and sacroiliac joint. Hence, it permits to manage both columns, with direct buttressing quadrilateral plate fractures if required. 3D-shaped acetabular plates were recently introduced to fix the periacetabular region and buttress the quadrilateral surface, but wide experiences and clinical results are lacking.5 In some cases to obtain a satisfactory reduction is necessary a second time surgery through posterior approach with additional plates. Therefore, the primary aim of the present study was to assess the efficacy of reduction using a single pre-shaped suprapectineal plate (Pelvic Pro System, Stryker®) by ilioinguinal approach with Stoppa window, in some specific acetabular fractures. The secondary aim was to demonstrate the effectiveness of using suprapectineal plate through with ilioinguinal approach with Stoppa window by evaluating the postoperative radiological and clinical results of patients who had a minimum 24- month follow-up.
MATERIALS AND METHODS
A total of 256 patients were treated surgically for acetabular fractures at our level 2 trauma hospital from January 2013 to February 2019. Medical records and radiographs were analyzed retrospectively. Inclusion criteria were: All patients who were treated surgically with anatomic suprapectineal plate for both-column pattern, the anterior column, posterior hemitransverse pattern, and the T-shaped pattern, involvement of quadrilateral plate and minimum 24-month follow up were included. Closed head injury that caused prolonged immobilization or history of ipsilateral hip injury, fracture with no involvement of quadrilateral plate, patients lost at follow-up and single Kocher-Langenbeck approach were excluded. Pre-operative computed tomography (CT) with 3D reconstruction were always performed to assess and classify fracture pattern. Our institutional review board approved the study and informed consent was obtained from all patients involved in the study.
All the cases followed the same post-operative rehabilitation protocol and were allowed to bear full weight 6 weeks after surgery. Patients were followed clinically and radiographically at 4 weeks, 3 months, 6 months and 1 year. Patients returned to clinic after a minimum of 24 months of follow-up for a re-evaluation, including physical examination, completion of quality of life surveys and radiographic examination. Functional status was assessed using visual analogue score (VAS), Harris hip score modified (HHS), Hip disability osteoarthritis outcomes score (HOOS) and Merle d’Aubigné score.
Operative technique
All patients were managed with similar surgical approach. CT scan and three-dimensional (3D) reconstruction and Doppler ultrasound of the pelvis and the lower extremities were routinely performed before and after surgery. The ilioinguinal approach with Stoppa window4 was performed by a senior surgeon (RP, RF, AV) in each case. Specifically, we extended the pelvic view of ileo- inguinal approach with a typical 10-cm horizontal Pfannenstiel incision two fingerbreadths superior to the pubic symphysis. Subsequently, we proceed to protect the spermatic cord or round ligament, to excise the emirectus insertion on the pubis, and to incise the transversalis fascia superior to the pubic symphysis to get access to the retropubic space of Retzius.6 Corona mortis, obturator nerve and femoral vascular bundle, were identified and protected during surgical procedures. After proper exposure, the reduction of the fracture was done under direct vision through pelvic clamp, K-wires or lag screws if necessary. 3D anatomical preshaped suprapectineal plate (Pelvic Pro System, Stryker®) along with the pelvic brim was applied to provide the main mechanical support for acetabular fracture fixation.
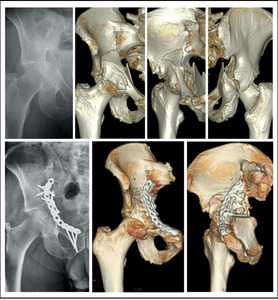
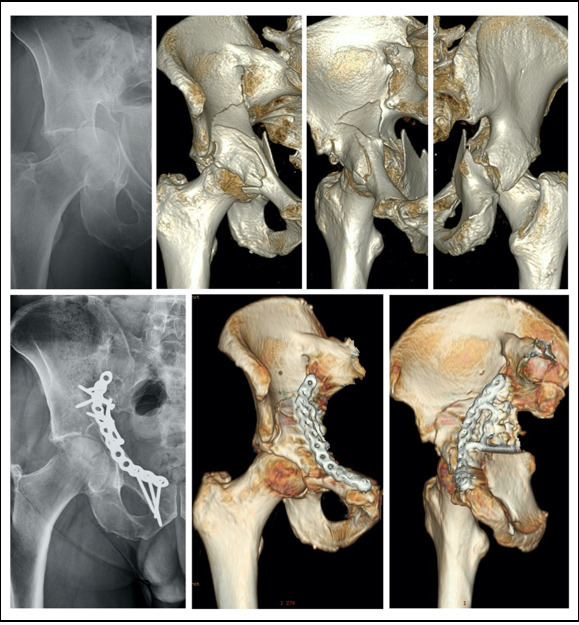
Within ten days from the surgery, a post-operative CT were performed to assess the quality of reduction of upper weight-bearing dome of the acetabulum in accordance to Matta’s criteria7 (Figure 1).
The Kocher-Langenbeck approach and additional plates were used in order to get anatomic reduction of posterior wall or column.
RESULTS
33 patients with complex acetabular fracture managed with an anatomic preshaped suprapectineal plate (Pelvic Pro System, Stryker®) were included in the study with a mean age of 59.09 years (range; 22-86). Average follow-up was 40.4 months (range; 24-73). Patient characteristics, fracture pattern, mechanism of injury, and associated injuries are shown in Table 1 and Table 2. There were no open fractures. The quadrilateral plate was involved in each case. The 82% of patients were treated only with a suprapectineal plate using ilioinguinal approach with Stoppa window (Figure 2). Of these, 22% of patients required the use of an additional plates due to iliac wing fractures. The 18% of patients required a Kocher-Langenbeck approach in order to get anatomic reduction of posterior wall or column.
Functional assessments, complications and quality of reduction of patients were summarized in Table 4. Deep infection of surgical wound was observed in 6% of patients. One patient was characterized by wound dehiscence occurring few days from surgery. The patient required intravenous antibiotics until resolution of infection. One patient was characterized by a late-onset deep surgical site infection that required antibiotic therapy and a second surgery to remove hardware after six mounths. A case of incisional hernia that required surgery, occurred. In 3% of patients, one vascular injury occurred during surgery. A vascular prosthesis required to control arterial bleeding.
Despite, the poor quality of reduction of 21% of patients assessed by post-operative CT, no re- operations were performed due to poor bone stock, acetabular bone loss and increased anesthesiologic risks.
DISCUSSION
Displaced complex acetabular fractures usually require open reduction and internal fixation, because of high incidence of unacceptable results following conservative treatment.8 The management of these fractures is laborious for trauma surgeon due to its deep location and complex anatomy. Moreover, fixation might become technically challenging in case of osteoporous bone. The cohort of the present study was characterized by an age range of 22 to 86 years. Indeed, it is known that complex acetabular fracture might occur following a high energy (i.e. car accident) or low energy trauma (i.e. simple fall) especially in case of frail, elderly and osteoporotic patients. For these reasons, additional injuries, comorbidities, bone quality, and surgical risk need to take into consideration in the diagnostic and therapeutic course of the patient.9
To our knowledge, there have been limited publications in the current literature about the techniques used in the management of complex acetabular fractures with quadrilateral plate involvement. The use of suprapectineal plating versus infrapectineal plating is still debated.10 It has been established that infrapectineal plating may help to prevent acetabular protrusion in case of quadrilateral plate involvement. Special attention should be given to protect urinary bladder and neurovascular structures encountered during subperiosteal dissection of quadrilateral plate.10 A recent study by Yucens et al11 indicated that infrapectineal fixation models with unlocked screws are much more stable than any suprapectineal application. At the same time, we need to consider that locked screws must be preferred in particularly osteoporotic patients.12 Therefore, suprapectineal plating with entirely locked screws represents the best choice of fixation in case of complex acetabular fractures following low energy trauma in osteoporotic aged patients.11
In the present study, we used a new anatomical plate characterized by both suprapectineal and infrapectineal holes due the 90° bent triangular component from the inner side of the main plate. This triangular plate component placed on quadrilateral surface connects the anterior column with the posterior one. In this way, we got the advantages of suprapectineal and infrapectineal plating in terms of reduction and stability. Moreover, we routinely placed an infra-acetabular long screw between both columns in order to achieve the goal of perfect reduction, compression and rigid fixation in case of complex acetabular fractures as illustrated by Culemann et al.13
Focusing on the clinical results, the present study showed that 91% of patients were satisfied of their condition during activity of day living and only a small cohort reported walking aids. Moreover, using the Merle D’Aubignè scoring system and HHS, respectively 85% and 82% of patients were rated good or excellent. Our results are in line with those of previous studies.14–17 Hirvensalo et a15 published the largest series with 164 patients. They found that 80% of patients achieved an HHS of 75 or greater on clinical examination. Sagi et al15 published that the 88% of patients using the Merle D’Aubignè scoring system were classified good or excellent. Laflamme et al16 reported that 92.9% and 70.6% of their patients were rated as good or excellent using respectively Merle D’Aubignè score and HHS. More recently, Sheng et al17 analyzing a similar cohort, reported that 87.5% of patients were rated good or excellent.
Regarding the quality of reduction, it is evident that CT is more accurate than plain radiography for evaluation of acetabular fracture reduction. Indeed, we reported that 18% of patients were re-operated to get optimal reduction of posterior column or wall despite the good reduction assessed by plain radiographs.19-21
It has been well established that when anatomical reduction is achieved especially in the upper weight-bearing dome of the acetabulum, an excellent or good functional outcome can be estimated in 83–89% of patients.18 In our series, according to Matta’s criteria, satisfactory reduction (anatomical and imperfect) has been achieved in 79% of patients. The results of large series of patients operated by the modified Stoppa approach have been reported by several authors.14,15,19 Sagi et al ,15 Andersen et al,19 and Hirvensalo et al14 reported respectively satisfactory reduction in 92%, 82% and 84% of patients.
Historically, two types of displacement (step and gap) have been proposed to evaluate the quality of reduction in the upper weight-bearing dome of the acetabulum. Verbeek et al. indicated that residual gap displacement appears better tolerated than step displacement in terms of hip survivorship and clinical outcomes.20 For instance, analyzing the results of reduction and clinical outcomes of patients classified as “poor reduction” (Table 4), we could observe that the worst clinical results were obtained in patient 1 characterized by highest step displacement.
Regarding complications, the Stoppa approach has been confirmed as a limited intra-pelvic approach associated with a decreased complication rate and significantly shorten operative time. Our complications rate and surgical time are comparable to those reported by others.16 It is worth noting that removing hardware due to infection has proven to be difficult and high demanding. Therefore, we advise to remove hardware only if strictly necessary. This study has several limitations due to its retrospective design and the lack of a comparative cohort.
CONCLUSION
In conclusion, the present study reported that only in a small cohort of patients, an additional posterior approach was required to get anatomic reduction. Furthermore, our results shed light on the outcomes of the specific use of new generation suprapectineal plate in complex fracture pattern in wide range age of patients.
Achnowledgments
None
Contributions
RB, RP, AV performed surgeries, study conceiving LF data analysis, manuscript writing - original draft; DP, LDB data collection
APG, assisted with the data interpretation; DC, SC methodology, manuscript revising.
Conflict of interest
The authors declare that they have no conflict of interest
Funding
None
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol, participant education and recruitment materials, and other requested documents — and any subsequent modifications — were reviewed and approved by the Department of clinical and molecular science (DISCLIMO) board in according to the Policy of Clinical Orthopaedics, Università Politecnica delle Marche, Ancona, Italy. To carry out the present study, the patients did not be exposed to additional doses of X-rays, because we meticulously reviewed radiological and medical chart
Informed consent
Informed consent was obtained from all individual participants included in the study.