INTRODUCTION
Life expectancy has significantly increased in recent decades, especially in industrialized countries, thus contributing to the emergence of new pathologic conditions. The most common worldwide age-related bone disorder is osteoporosis1 which consists of a generalized reduction in bone mass with alteration of the bone microarchitecture.2
It is estimated that osteoporosis in Italy affects about 5,000,000 people, 80% of which are postmenopausal women.3
Osteoporosis is one of the conditions that predispose to fragility fractures. The pathophysiology of fragility fractures is the discrepancy between the strength of bone and the amount of load put on it.4 Fragility fractures can be caused by low-energy trauma that would not be sufficient to fracture healthy bone or can be caused by physiologic load,5 such as fragility fractures of the pelvis (FFP) and particularly fragility fractures of the sacrum (FFS).6–8
FFS occurs following simple domestic falls from standing position or even sitting position; sometimes the patient does not remember the traumatic event. This often leads to an underestimation of symptoms and a consequent delay in diagnosis. In recent years there has been an increase in prevalence of FFP and FFS related to the high life expectancy and to better imaging.9 Besides, a gross calculation estimated that the numbers will triple by the year 2030.10 In addition to osteoporosis, other factors can predispose the development of FFS; local bone alteration due to tumors or radiotherapy11 as well as biomechanical factors such as hyperlordotic posture, relaxation of the pelvic ligaments, long-term immobilization and overweight play an important role.12 Pregnancy and lactation leading to secondary osteoporosis were also reported to cause FFS.13,14 Degenerative spondylolisthesis on level L5/S1 can also determine FFS by increasing the shear forces on the endplate of S1.15 Finally, spinal instrumentation is also an important risk factor for FFS.16 According to Morris et al,17 the most important risk factor for fragility fracture is a previous fragility fracture. For this reason, orthopaedic community has a unique opportunity to prevent further fractures by determining the appropriate medication and initiating treatment.
DEFINITION
There is still some confusion in the literature regarding the nomenclature of the different type of fractures. Rommens et al.4 used the term “fragility fractures” as synonyms of osteoporotic, insufficiency and stress fracture. However, these types of fracture show substantial differences. Both in fragility fractures and in insufficiency fractures the substrate is made up of abnormal bone, but in the first one it is still possible to recognize a low-energy trauma as the cause. Conversely, insufficiency fractures are due to bone modification that result in an inability of the bone to resist physiological loads, thus the body weight can be sufficient to produce a fracture. Irradiation, long-term immobilization, long-term cortisone intake are some of the risk factors for insufficiency fractures.18–20 Nonetheless, some authors use the terms “fragility fracture” and “insufficiency fractures” as synonyms.21
Stress fractures have to be considered as a separate entity. According to Matcuk et al.22 stress fracture is the result of abnormal load upon normal bone, while insufficiency fracture is the result of normal loading upon abnormal bone. Stress fractures are seen in bone with a normal structure and strength, which is set under repetitive peak loads. These are caused by repeated stresses rather than direct trauma. The most common stress fractures affect proximal tibia, distal fibula, metatarsal bones, navicular bone and the neck of the femur.23 The sacrum can also be affected by stress fracture, most commonly in young female runners.24 Stress fractures typically occur in younger patients more frequently than fragility or insufficiency fractures.
CLASSIFICATION
The mechanism of injury for fragility fractures of the sacrum differs from those occurring in young active patients, usually due to high energy traumas. The latter are usually classified according to Denis et al.25 Fractures lateral to the sacral foramina are classified as zone I and represent about 50% of the patients. When the fracture involves the neural foramina but does not involve the spinal canal is referred as zone II, while if medial to the neural foramen, involving the spinal canal is zone III. Additionally, Roy-Camille et al.26 described another pattern of fracture named “suicidal jumper’s fracture”, in which there is a transverse fracture line in addition to bilateral sacral fractures, thus causing a spinopelvic dissociation with protrusion of the lumbar spine into the pelvis. Recently, Wagner et al.27 reported on sacral bone mass distribution and corresponding changes with decreased general bone mass. They found that paraforaminal lateral region (zone I) is the area with the lowest bone mass, and decreased bone mass at S2 compared with S1. This explains the specific patterns of fracture that occur in FFS, with fractures lines located in the Denis zone I, and also the horizontal fracture line between S1 and S2, not uncommonly seen in FFS.28 These “H-type” fractures have been found in 21% of FFS in a series of 245 patients with a FFP.4
Due to the differences in the mechanism of trauma, hemodynamic condition, clinical signs and symptoms, bone density and patterns of fractures, Rommens et al.4 proposed a new specific classification for FFP based on analysis of conventional radiographs and CT scans. Even though it has not yet been validated, it provides hints for treatment strategies and is widely used, as it is based on morphological criteria and corresponds to the degree of instability. FFP Type I lesions include anterior pelvic ring fractures only; FFP Type Ia is unilateral, whereas Type Ib is bilateral. FFP Type II lesions are non-displaced posterior lesions; FFP Type IIa is a non-displaced posterior lesion only, whereas FFP Type IIb is a sacral crush with anterior disruption, and FFP Type IIc is a non-displaced sacral, sacroiliac or iliac fracture with anterior disruption. FFP Type III lesions are characterized by a displaced unilateral posterior injury combined with an anterior pelvic ring lesion; FFP Type IIIa involves a displaced unilateral ilium fracture; FFP Type IIIb is a displaced unilateral sacroiliac disruption; and FFP Type IIIc is a displaced unilateral sacral fracture. FFP Type IV lesions are characterized by displaced bilateral posterior injuries; FFP Type IVa has bilateral iliac fractures or bilateral sacroiliac disruptions; FFP Type IVb is characterized by a spinopelvic dissociation containing a bilateral vertical fracture through the lateral mass of the sacrum with a horizontal component connecting them (a U- or H-type sacral fracture); and FFP Type IVc is a combination of different posterior instabilities.29
CLINICAL PRESENTATION
When approaching to an elderly patient with low back pain, groin pain or pain to the pubic region, physicians need to take into consideration the possibility of a FFS or a FFP. In addition to pain, patients usually suffer from significant reduction in mobility, as pain is typically exacerbated while weight-bearing and improves while at rest.12
Weber et al.30 in a 2-year prospective study found the frequency of FFS in women aged over 55 years who presented at the emergency room for low back pain to be 1.8%. Unfortunately, due to limited knowledge on these disease, they are often underestimated. As a result, patients are often treated for low back pain without a proper diagnosis.31
Typically, the injury mechanism consists of a low-energy trauma: a domestic fall from a standing or sitting position. Some patients do not even remember any trauma. It is important in those patients to meticulously collect the clinical history, as very often patients have history of osteoporosis or fragility fractures in other districts. Additionally, they often assumed cortisone for long periods or have history of irradiation for malignant tumor in the pelvis.
An accurate physical examination can guide the physician to the correct diagnosis. Sacral tenderness on lateral compression, sacroiliac joint tests, hip flexion-abduction-external rotation (FABER) test, Gaenslen’s test and squish test, although not specific for FFS, are often positive.12
Patients with FFS often sustained no major injuries to soft tissues and are hemodynamically stable in the acute setting.4 However, hemodynamic instability can occur over time, especially in patients that assume anticoagulants for concomitant cardiovascular co-morbidities. For this reason it is important to monitor those patients for at least 24 hours on a monitoring ward or a critical care ward.32
IMAGING
A diagnostic algorithm was proposed in 2015 and it is the same adopted in our institution (Fig. 1).21 The first imaging modality to investigate a patient with a suspected fragility fracture of the sacrum is conventional radiology of the pelvis in the antero-posterior view. Fractures of the superior and inferior pubic rami or the pubic bone are easily recognized with these radiograms. However, due to the low density of the bone, especially in the elderly patient, and the superimposition of the bowel content and bladder it is very common to not recognize a fracture in the posterior ring.33 Moreover, sacral fractures are also referred in the literature as “occult fractures”, and they can be seen in the radiographs as sclerotic bands, cortical disruptions or fracture lines.34 However, in most cases they remain unseen on conventional radiographs. As a result, the role of the conventional radiographs in the diagnosis of FFS is minimal and their mainly used to exclude other pelvic fractures or other pathologies that could enter in the differential diagnosis. In addition, it is very common that an anterior pelvic ring fracture is associated with a FFS; therefore, a second-level imaging modality should be prescribed in such cases.4
Henes et al.35 compared diagnostic accuracy of magnetic resonance imaging (MRI) and of computed tomography (CT) in the detection of pelvic fractures. MRI proved to be significantly better compared to CT, particularly in the depiction of fractures of the sacrum, reaching a sensitivity of 98.6% compared to 66.1% in CT scans. This probably because sometimes FFS are occult and without cortical disruption. MRI, in particular utilizing either STIR, T1-weighted, or fat-saturated T2-weighted fast spin-echo sequences is able to detect small cancellous bone fractures, bone edema and bleeding.
Bone scan is one of the most sensitive imaging modalities and it was considered the gold standard for detecting FFS for many years. However, with the advent of MRI being widely available in recent times, its usefulness is limited in the diagnosis of FFS.
In a recent study, Kim et al.36 showed that FFS are more commonly diagnosed on lumbar spine MRI than with any other non-lumbar imaging modalities, such as pelvic MRI, pelvic CT or bone scan. This is because FFS frequently mimics lumbar spine pathology and different causes of pain.
TREATMENT
Patients affected by FFS are often fragile and with other comorbidities that needs a multidisciplinary team of orthopaedic trauma surgeons, geriatricians, pain therapists and physiotherapists, in order to optimize the treatment algorithm.37 Undoubtedly, the first step is to optimize the general conditions of the patients as soon as possible and to keep monitoring the vital parameters during the whole hospital stay and after.
Choosing to treat the patient either conservatively or surgically should be based on general health status and on the activity level of patient prior to injury.
The main goal of treatment of FFS is similar to that of hip fractures: early mobilization and weightbearing, efficient pain relief and early discharge from the hospital to a proper facility for rehabilitation.38 Ensuring the highest possible degree of independence for the patient is more important than anatomical reduction and restoration of pelvic symmetry.
Conservative treatment
Rommens and Hofmann,4 on describing the classification for FFP, also provided recommendations for surgical treatment. They suggested conservative approach when only the anterior ring is involved (type I), while surgical fixation need to be considered when the posterior pelvic ring and the sacrum are involved, since with early mobilization there is a risk of increasing instability or nonunion.
Treatment of non-displaced sacral fractures (type IIc) is still controversial even though they represent the most common pelvic fracture pattern in elderly patients.21 In the past, the approach to these fractures was bed rest and immobilization for prolonged times. However, it has been shown, especially in elderly patient, that this approach leads to many other immobility-related complications, such as deep vein thrombosis and pulmonary embolism, pneumonia, urinary tract infections or side effects of prolonged non-steroidal anti-inflammatory drug (NSAID) therapy.39 Nowadays, this strict conservative approach is not tolerable anymore. Conservative treatment of these patients requires early mobilization. As suggested by Rommens et al.,29 patients with non-displaced FFS that usually present with pain in the dorsal pelvis and often also in the groin due to associated pubic rami fractures need adequate pain medication from the first days of hospitalization. Indeed, due to acute and intense pain it is often impossible to mobilize them early. If no pain relief can be observed within one week, or when mobilization is apparently difficult, surgical treatment should be conidered. Moreover, it is important to repeat the x-rays and CT scan of the pelvis after early mobilization in order to rule out further fracture displacement.
Surgical treatment
Operative treatment is recommended in every displaced unilateral and bilateral fracture of the sacrum (Type IIIc and IV b-c).29 However, no clinical evidence has been provided with adequate level of evidence and most of surgical indications still rely on expert opinions.21
Sacral stabilization of FFS in elderly has different aspect to consider compared to the high-energy fractures typical of young people. Patients often have multiple comorbidities and a minimally-invasive technique has to be preferred. Additionally, bone quality is usually osteoporotic, causing a higher risk of failure of the implants.
Any anterior instability must be recognized and eventually treated in combination with the sacrum. Moreover, in such cases, stabilizing only the posterior ring leads to a higher risk of implant loosening or secondary displacement.40
Several less-invasive techniques have been proposed in the last years for posterior pelvic fixation, albeit there is no evidence of superiority of one over another and only case series have been published, ultimately recommending the described procedure. Nevertheless, the tendency that can be safely deducted from the literature is the shifting that has occurred in recent years from open procedures with internal fixation towards closed internal fixation techniques.40
Ilio-sacral screw osteosynthesis
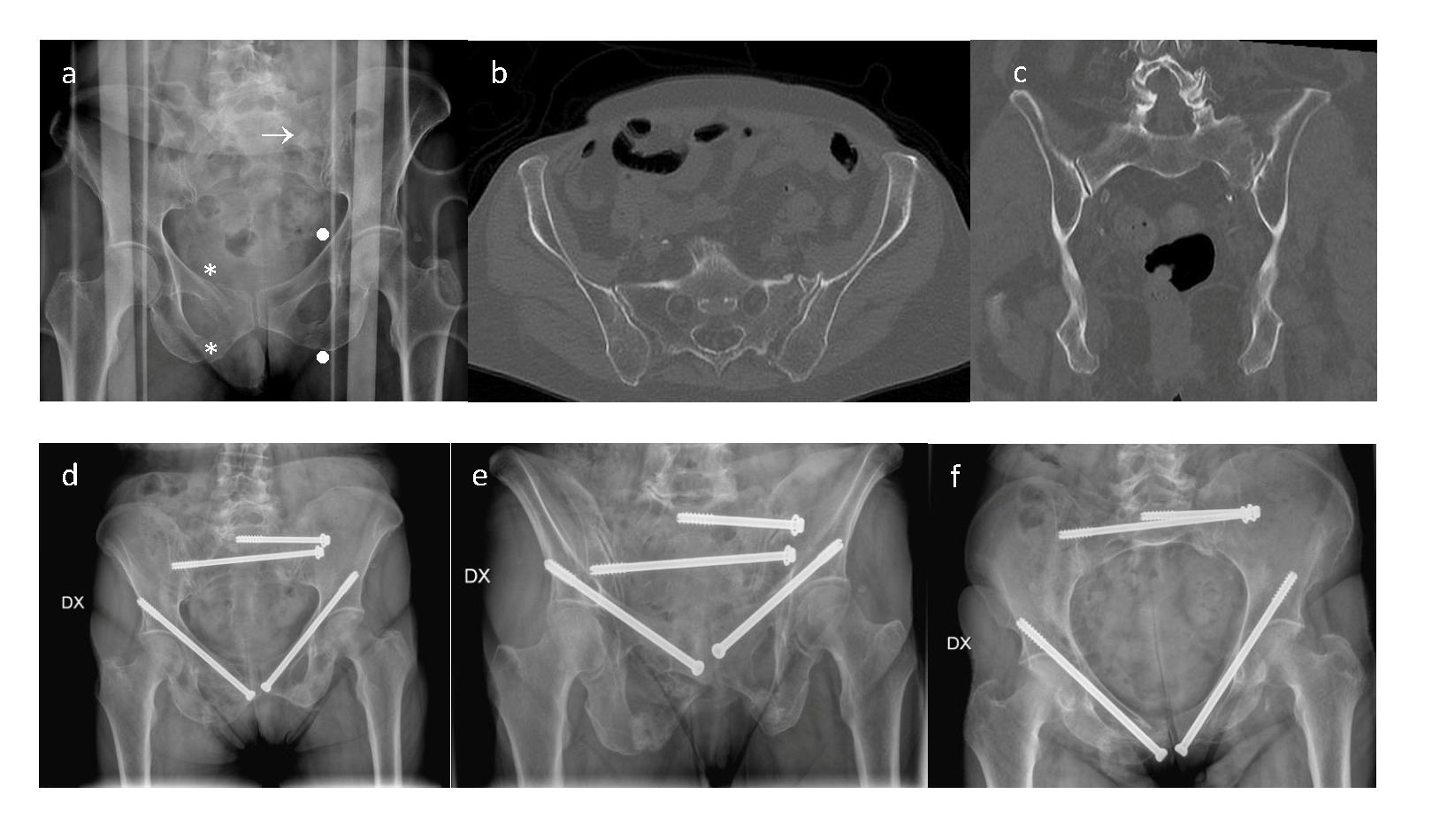
Percutaneous ilio-sacral screw fixation has been reported to be a valid surgical technique to fix non-displaced fragility fractures of the sacrum.12,37 It is recommended to insert two fragment screws into the body of S1 or one screw into the body of S1 and S2 each. Mechanical stability achieved with two screws as compared to only one screw has been shown to be significantly higher41 (Fig. 2).
As the bone mineral density is low in these patients, this technique has a potential higher risk of loosening because of a lower pull-out force of these screws.42 Furthermore, cemented augmentation of this screws has been proposed in order to provide higher pull-out forces. A systematic review on 11 studies recently compared augmented versus non-augmented ilio-sacral screws.43 Cement augmented techniques proved to have better biomechanical properties in vitro in terms of pull-out forces and construct stiffness, albeit only few clinical case series, with no control groups and relatively low numbers of patients confirm the method to be safe and effective.6,44,45
Recently, a new alternative screw design was proposed adopting the so-called screw-in-screw implant prototype for fragility sacrum fractures fixation, intending to increase the resistance against rotation via two-point fixation in the sacrum.46 However, no clinical studies were performed yet.
Closed reduction and internal fixation of the sacrum with screws has been reported to be technically challenging and radiation intense, with reported screw misplacement rates ranging from 2.8% to 29.5% when conventional 2D fluoroscopy-based approach was used.47–50 Recently, many institutions have implemented the possibility of having 3D image-guidance technology in the operating room, with high performing devices that provides excellent imaging quality. Moreover, 3D image-guidance accuracy has been shown to be 99.2%47
Sacroplasty
The first study reporting the possibility of treating isolated sacral ala fractures (type IIa) with sacroplasty was published in 2002 by Garant et al.51 This procedure, similar to vertebroplasty and kyphoplasty, consists in the injection of polymethylmethacrylate (PMMA) into the cancellous bone under imaging guidance. Typically, the level of injection is at S1 and S2, as they provide the greatest amount of stability to the sacrum and are often involved in the fracture pattern.52 The goal of the procedure is to relieve pain through restoration of mechanical integrity. The main complication that can occur during the procedure is cement extravasation. A recent systematic review53 looked for safety and efficacy of sacroplasty, showing that cement leakage was often reported as a complication but in most of the cases was clinically insignificant. The authors also confirmed that sacroplasty is effective in relieving pain. However, most studies included in the review reported only short-term follow-ups (one month to one year),53 and then long-term outcome of the procedure remains unknown.
Trans-sacral bar osteosynthesis
Trans-sacral bar osteosynthesis technique has been proposed for fixation of FFS to provide an adequate interfragmentary compression, which is hard to achieve with cancellous sacroiliac screws due to low bone quality in the sacral body. The procedure consists in placing a 6-mm threaded bar in sacral corridor of S1 or S2, perpendicular and through the fracture plane. Then washers and nuts are placed at both sides over the bar. Tightening of the nuts creates compression in the fracture gap.54 Intraosseous trans-sacral corridors are safe pathways where to put the bar to avoid neurological or vascular damage. It has been demonstrated that there is consistent variability in their dimension and not all individuals are amenable to trans-sacral fixation.55 In a 3D CT model study on 156 adults’pelvic CT scans, trans-sacral implant positioning was critical (<12 mm of maximum diameter) in 52% of cases for S1 and 21% for S2, and impossible (<8 mm) in 26% for S1, with no impossible corridor for S2.55 This showcases that a thorough anatomical knowledge and preoperative planning are mandatory using trans-sacral implants.
Nevertheless, when the anatomy of the sacrum is favorable, combination of trans-sacral screws and ilio-sacral screws provide higher load to failure and reduced fracture displacement, as demonstrated in a biomechanical study.56
Although no large prospective cohort studies were published, some small case series showed promising results in terms of clinical outcomes of trans-sacral bar osteosynthesis for the treatment FFS.54,57
Lumbo-pelvic fixation
Complete dissociation between the pelvic ring and the ilio-lumbar spine corresponds to type 4 FFP. These injuries have the greatest degree of instability and therefore open surgery is recommended.40 Spino-pelvic fixation is the technique of choice, especially for U-shaped or H-shaped sacral fractures58 and for patients with critical dimension of trans-sacral corridor27,29 (Fig. 3). This technique involves bilateral placement of a proximal pedicle screw at the level of L4 and/or L5 and a distal pedicle screw on the posterior surface of the ilium. The two screws are then connected through a bar on each side and the two bars are connected with a transverse connector.59 To ensure greater stability, the procedure can be implemented by adding a trans-sacral screw or a trans-sacral positioning bar to form the so-called triangular osteosynthesis.
The technique requires extensive surgical exposure, which is associated with high risk of blood loss and infection.59 In recent years, a percutaneous technique has been proposed to reduce the risk of complications60 (Fig. 4).
SUMMARY
Attention must be paid in elderly patient who suffer from a low-trauma energy in order to not miss the diagnosis of a FFS. A careful clinical history must be harvested and clinical examination is fundamental to raise the suspicion. Any pain in the lower back or in the groin must be investigated with conventional radiographs, but cross-sectional imaging is often needed to exclude FFS in patients with persistent low back pain during mobilization. Patients with FFS must be mobilized as early as possible. Most of the times non-operative treatment is suitable with adequate pain management. Operative treatment is recommended when pain is not tolerated during mobilization or when the fracture pattern is unstable, with a high risk of progression and further displacement. Less invasive techniques have to be preferred over open reduction and internal fixation as patients are often fragile and with comorbidities.
ACKNOWLEDGEMENTS
None
AUTHORS’ CONTRIBUTION
The authors contributed equally
FUNDING
None
CONFLICT OF INTEREST STATEMENT
All authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations and grants or other funding.
HUMAN AND ANIMAL RIGHT
For this type of study is not required any statement relating to studies on humans and animals.