Introduction
Hip fracture in the elderly patient is an adverse event related to high mortality at one month and at one year and with an important impact on the quality of life of patients, resulting in disability that can be permanent with loss of self-sufficiency.1,2 The percentage of elderly people in Italy is very high, people aged >65 make up 22.8% of the total population, with 2.2 million of elderly people (age >85 years old),3 which is estimated to represent more than 12% of the population in 2050.1 In addition, Italy is one of the countries with the highest incidence of femur fractures recorded annually per 100000 inhabitants, with an incidence >300 for women and >150 for men.4 Between 2012 and 2019, our country has recorded an increase in surgical admissions for femur fractures, quantifiable in almost 10,000 interventions: from 84,698 in 2012 to 94,643 in 2019.5 This may be related to an increase on life expectancy caused by improved care and quality of life. However, the increase in the number of older people also leads to an increase in the frequency of age-related diseases such as osteoporosis. With the increase in population aging, it is globally expected that the number of femur fractures will continue to increase, thus rising from 1.26 million events recorded in 1990 to 4.5 million in 2050.6 In addition to the fracture, even the subsequent surgery turns out to be a traumatic event in the elderly patient also for the possible multiple comorbidities. It is therefore very important to reduce the risk of complications as much as possible. Among these complications is perioperative anemia with the subsequent possible need for blood transfusion,7,8 which is related to risk factors such as: age, low haemoglobin at admission, increased international normalized ratio (INR) at admission, female gender.9 In order to prevent this complication the use of local or i.v. antihemorrhagic drugs may be considered. Among these, both tranexamic acid, one of the most widely used,10 and fibrin sealant11–20 have proven to be effective in reducing postoperative anemia, blood loss, the need for transfusion, and blood volume in the drainage. The latter has already been shown to be effective in reducing blood loss in vascular surgery, abdominal surgery, liver surgery, and ENT surgery21,22 and has also been evaluated in patients undergoing hip hemiarthroplasty for femoral neck fracture in which a reduction in the need for transfusion and mean transfused volume was demonstrated.23 The aim of our study was to evaluate the efficacy of fibrin sealant and the tranexamic acid in reducing the need for blood transfusion in elderly patients undergoing partial hip replacement surgery following femoral neck fracture and to compare it with the use of post-operative drain or with standard hemostasis.
Patients and methods
The study was approved by the Ethical Committee of Catholic University, Rome. The approval number of this retrospective study is (N. 0009156/21). All data were collected at patients’ visit to the clinic and used anonymously. In our study, all patients admitted to the Orthopedics and Traumatology department of the A. Gemelli Polyclinic with a diagnosis of proximal femur fracture from September 2018 to March 2021 were involved. Inclusion criteria were: diagnosis of femoral neck fracture, classified as AO 31B2-3,24 surgical treatment with hip hemiarthroplasty performed with the same surgical approach, hemoglobinemia on admission > 8 gr/dL. Exclusion criteria were: previous surgery on the affected hip, coagulation disorders, hematopoietic disorders, advanced renal failure (grade IV and V) undergoing dialysis treatment. Patients were divided in four groups depending on the use of haemostatic agents. The first group (EVICEL group) included patients who were administered a fibrin sealant as a local haemostatic; the second group (TRANEX group) included patients who were administered an antifibrinolytic; in the third group (drain group) were included patients who had had a post-surgical drain placed; the other patients, who were treated with standard haemostatic care, were included in the fourth group (control group). In our protocol, each patient underwent partial hip replacement surgery performed by an orthopedic surgeon experienced in traumatology. Each patient was given a Cefazolin 2g dose as antibiotic pre-operative prophylaxis, if not contraindicated and in all cases a posterolateral approach was used. After the removal of the femoral head and the regularization of the femoral neck osteotomy, the prosthesis was implanted according to the manufacturer technique. Subsequently, 4 ml of EVI-CEL (EMEA/H/C/0 0 0898, Omrix Biopharmaceuticals N. V., Diegem, Belgium) were sprayed on the soft tissues of patients included in the EVICEL group. EVICEL is presented in two separate frozen vials. After a one-hour thawing, 4 vials (2 vials for each component, 4 ml total) where applied with a sterile administrative device, specifically designed to diffusely spray the components in equal quantities. The two components activate on contact with each other, reaching the tissues in their active form. Among the various fibrin sealants available in the market, EVICEL (Omrix Biopharmaceuticals N. V., Diegem, Belgium) was chosen because of its more favorable mechanical, kinetic, and biochemical properties.25,26 In the TRANEX group, after implant positioning, 1 g of tranexamic acid (Acido Tranexamico Bioindustria Lim, Biondustria Laboratorio Italiano Medicinali S.p.A., Novi Ligure, Italia) was administered intra articular. Tranexamic acid is presented in 500 mg/5 ml vials and its use is indicated for the prevention and the treatment of major surgery bleeding. In the “drain” group post-surgical drainage was placed in order to avoid post-surgical hematoma formation. This drain (Pvc material, Ch 12-4 mm) was positioned below the fascia lata and was used in suction. Its removal was carried out 24 hours after the end of the surgery. In the control group, standard haemostasis care was performed. Wound closure was performed with simple sutures with the same technique in all patients. From the first postoperative day, patients began a rehabilitation program in which partial weight bearing was allowed. Of each patient involved, age, sex, weight, BMI height, comorbidities by modified Charlson Comorbidity index,27 intake of antiplatelet and anticoagulant drugs, INR at admission, duration of surgery, the number and volume of units of concentrated red blood cells transfused in the perioperative period, hemoglobin and hematocrit concentration at admission, in the first, third and fifth postoperative day were recorded. Low molecular weight heparin was administered every day for at least 45 days after surgery as antithrombotic prophylaxis.
The main outcome of our study was the need for concentrated blood transfusions in the 24 hours prior to the surgical procedure and over the next five days. The transfusion of concentrated emation is decided by the anesthetist during the surgery and during the hospitalization in post-operative intensive care and by the orthopedist during the patient’s stay in the ward. Secondary outcomes were: mean volume of blood transfused for each patient, variations in hemoglobin concentration and hematocrit and total blood loss. Blood loss was calculated using the formula proposed by Nadler et al28 for the determination of total blood volume. This data was included in the formula proposed by Ward for the estimation of blood losses,29 corrected for blood replacement by transfusion as described by Sehat.30 The formula used was: GBL = EBV ln Htci/Htcf +VT, GBL: global blood loss, EBV: estimated blood volume, Htc f: post-operative haematocrit; Htc i: haematocrit on admission, TV: transfused volume
Statistics
Data were registered on an Excel spreadsheet (Microsoft, Redmond, USA) and analysed usingR (version 4.1.2, R Foundation for Statistical Computing, Vienna, Austria).31 Data were described as mean and standard deviation for interval variables and as absolute numbers and relative frequencies for nominal variables. Comparison between groups was performed with chi-square test for nominal variables. When a significant difference was found, a post-hoc analysis with a pairwise Fisher exact test was performed. Normal distribution of interval variables was assessed with a Shapiro-Wilk test. Associations between nominal and normally distributed interval variables were assessed with ANOVA. In case a significant difference was found, a post-hoc analysis was performed with Tukey test. For non normally distributed variables, Kruskal-Wallis Significance was attributed to a p value < 0.05
Results
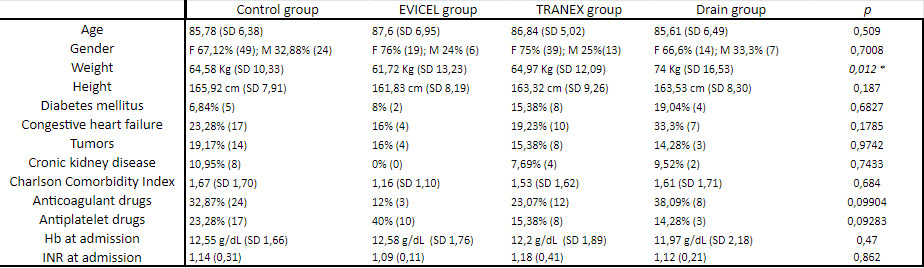
From September 2018 to March 2021 171 consecutive patients were admitted to our department32 with a diagnosis of femoral neck fracture AO 31B2-3 and were enrolled in our study. There were 121 females (70,77%) and 50 males (29,23%). 47 patients (27,48%) assumed anticoagulant drugs, while 38 patients (72,52%) assumed antiplatelet drugs. EVICEL was used on 25 patients, who were included in “EVICEL group”, TRANEX was used on 52 patients, who were included in the “TRANEX group”, standard hemostatic care was used on 73 patients, included in the “control group”, while post-surgical drain was used on 21 patients, included in “drain group”. Mean age in EVICEL group was 87,6 ± 6,95 years, in the TRANEX group was 86,84 ± 5,02 years, in the control group was 85,78 ± 6,38 years while in the drain group was 85,61 ± 6,49 years. Baseline patient’s characteristics are described in Table 1. The only statistically significant difference in baseline characteristic between groups was the weight (p 0,012).
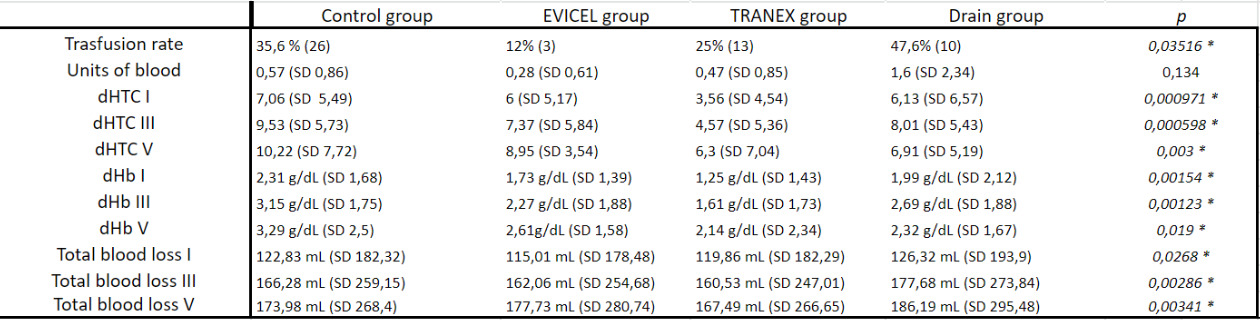
52 patients (30,4%) needed perioperative transfusion. 3 patients (12%) were transfused in the EVICEL group while 26 patients (35,6%) were transfused in the control group (p 0,0404). There was also statistical significant difference in the need of perioperative transfusion between EVICEL group and drain group with 10 patients (47,6%) transfused (p 0,0102). No differences were found between EVICEL group and TRANEX group (p 1).
Data regarding haematocrit and haemoglobin were available for all patient pre-operatively, in the first, in the third and in the fifth post-operative day. No significant difference could be found between TRANEX group and EVICEL group in terms of haematocrit and haemoglobin variation in the first, third and fifth post-operative day. Statistical significant differences was found about haemoglobin variation in the first post-operative day between TRANEX group and control group (p 0,000155) and between TRANEX group and drain group (p 0,013) and also between TRANEX group and control group in the third post-operative day (p 0,0004). Furthermore no statistical significant differences was found regarding haematocrit and haemoglobin variation in first, third and fifth post-operative day between EVICEL group and control group and between drain group and control group.
Differences was found about total blood loss between TRANEX group and control group (p 0,0052 in the first post-operative day, p 0,00035 in the third post-operative day and p 0,00069 in the fifth post-operative day) and between TRANEX group and drain group (p 0,0319 in the first post-operative day and p 0,0298 in the third post-operative day). The mean of blood loss in fifth post-operative day in control group was 173,98 ± 268,4 mL while in the EVICEL group was 177,73 ± 280,74 mL (p 0,0172). No significant difference could be found between TRANEX and EVICEL group in terms of total blood loss in first, third, fifth post-operative day (p 0,238; p 0,283; p 0,819) and also between EVICEL group and control group and between drain group and control group. Results are reported in Table 2.
Discussion
Anemia holds a very important role in geriatric population and represents of the predictive factors of poor outcome after hip fracture33–35 influencing short and long-term mortality, in addition to the length of stay, amount of blood transfusions, repeated hospitalizations, post-operative complications, poor functioning and a reduced quality of life.36
The main finding of this study is that the use that both of a fibrin sealant or tranexamic acid in a group of patients treated with hip hemiarthroplasty for intracapsular femur fracture reduces the need for transfusions and the transfused volume. Seven studies14–20 reported the outcomes of the use of a fibrin sealant during total hip replacement, while many studies confirm the protective role of tranexamic acid in bleeding control and avoiding blood transfusion.37–39
Crawford and colleagues20 reported a reduction of blood transfusion on a population of patients undergoing total hip arthroplasty for osteoarthritis. Zhao40 and Wang13 confirmed these findings in their metanalysis of 336 patients. Dae-Kyung et al39 confirmed in their study about the use of tranexamic acid in hemiarthroplasties the reduced need of blood loss and transfusions in the TXA group compared to the control group. In the present study, 30,4% of patients needed blood transfusions. 50% of them were administered to the control group, while 19, 2% occurred in the drain group and only 5,7% in the fibrin sealant group, while no difference was found between tranexamic acid and fibrin sealant itself.
The use of fibrin sealant reported a decrease in blood loss on total hip replacement23,25–27,29 as well as the use of tranexamic acid37–39 in both hip hemiarthroplasties and trauma surgery. We evaluated the total blood loss with a calculated estimation based on patients’ anthropometric parameters and variations in haematological laboratory results. The use of formulas to approximate blood loss during surgery were proved to be accurate and reliable.30 Randelli et al18 reported less haemoglobin and haematocrit decrease in patients who were administered a fibrin sealant, and the same result is confirmed in our study. Ashkeazi and colleagues41 in their study of 1722 patients who underwent hemiarthroplasty confirmed the inferior blood loss and transfusion need compared to the non TXA group. A more specific study conducted by Nissenhotlz et al33 on proximal femur fractures treated with hemiarthroplasty confirmed this trend.
A multicentre randomized trial compares the efficacy of a fibrin sealant, tranexamic acid and standard haemostasis in patients affected by subcapital femoral fracture.42 It concluded that tranexamic acid reduces total blood loss and hidden blood loss compared to fibrin sealant and standard haemostasis. No difference could be found in blood loss collected by drains and transfusion rate. No difference between TXA and fibrin sealant were detected in this study regarding total blood loss. Jordan and associates42 included both total hip replacements and hemiarthroplasties but patients with a history of myocardial infarction and thrombogenic arrhythmias and patients with cardiovascular stents and treated with anticoagulant or antiplatelet drugs were excluded. In the present study, 38,84% of patients assumed anticoagulant drugs, 31,40% assumed antiplatelet drugs, while the rest of the studied population (29,75%) did not assume neither of them. We included these categories of patients in the study because they represent a large part of the population of patients with a femoral neck fracture, improving the generalizability of the results. Moreover, we hypothesized that multimorbid patients would benefit most from the application of a fibrin sealant or TXA because of their comorbidities. In our institution, EVICEL (Omrix Biopharmaceuticals N. V., Diegem, Belgium) was chosen because of its mechanical, kinetic, and biochemical properties.26,27 IWe sprayed the fibrin sealant after the prosthetic implant as recommended by the manufacturer. This study has some limitations. The main one is the lack of randomization and its retrospective nature: the choice to administer EVICEL or TXA to patients was left to the operating surgeon, based on his personal preferences. It is impossible to completely exclude confoundants due to the extreme heterogeneity of the four groups and due to the scarce use of fibrin sealants in our daily practice, a disproportion exists in the numerosity of the study groups. Although drain tube is nowadays a less used tool to guarantee bleeding control, this is the only study in literature that compares four groups of patients with drain tube included in the comparison process.
Conclusion
In conclusion, this study demonstrates that the use of both fibrin sealant or TXA can reduce total blood loss and the need of transfusions in geriatric population with intracapsular femur fracture and consequently reduce complications due to prolonged hospital stays in the delicate post-surgical recovery.
Author contributions
The authors contributed equally.
Conflict of interests
The authors declare nopotential conflict of interest.
Funding
The authors received no financial support for the research and/or authorship of this article.