Introduction
Subtrochanteric fractures account for 10-35% of the proximal fractures of the femur.1
Due to the predominance of cortical bone, this region presents a weaker vascularization than the trans trochanteric region, which makes more difficult the healing of the fracture. (Figure 1)
Complex fractures with medial support failure present high rates of fixation failure and reoperation.2
Due to the anatomical features of the subtrochanteric region, the treatment of these fractures remains challenging.1,3
Over the years have been developed many classification systems for subtrochanteric femur fractures. The Russell-Taylor classification is based on involvement of the lesser trochanter and fracture extension up to the piriformis fossa and is primarily used in our study.4
Operative management of subtrochanteric fractures is the main treatment. Intramedullary nails (IM) and extramedullary plates are the first surgical implant options. Of these, IM nails have a biologic and biomechanical superiority, and in years have become the gold standard (Figure 2).5,6
Today the use of IM nail is a minimal invasive technique allowing for short skin incisions and less blood loss compared with other techniques requiring more surgical exposure, reduced infection rate, minimal tissue damage, a shorter operating time and early weight bearing.7,8 The use of a short rather than a long nail is still debated in literature.9
Operative complications of subtrochanteric fractures include malunion, nonunion, infection, implant breakage and their incidence reached up to 25%. Mortality rates at one year have been shown to be approximately 27%,with an increase in recent years due to the recent Covid 19 pandemic.10,11
Aim of this study is to retrospectively compare clinical and radiographic outcome of subtrochanteric fractures treated by long and short intramedullary nailing, analysing rates of complications in term of malunions, non-union, implant breakages.
Ethical Considerations
The institutional review board of the involved hospitals decided that no ethical approval was necessary as it was thought that for this retrospective study the informed consent of the patients was sufficient.
Materials and Methods
390 patients were chosen from the archives recorded into Orthopaedics and Traumatology departments of the IRCCS San Matteo hospital in Pavia and Edoardo Agnelli Hospital-Pinerolo (TO).
All patients suffered from a subtrochanteric fracture and were treated with intramedullary nailing between January 2010 and December 2019.
Inclusion criteria was clinical and radiological follow-up of at least 12 months. At the time of the evaluation 35 patients were dead and 16 did not compete the follow-up. 194 patients were available for the examination.
70 treated with a short intramedullary nail (Group A) and 124 with a long intramedullary nail (Group B).
Radiographic evaluation was performed at 6 and 12 months after surgery, in order to assess the presence of failure of the osteosynthesis. Clinical outcomes were evaluated by the return to normal activities prior trauma and VAS scale at mean follow up of 17.4 months (12-108 months).
Group A
Mean age at the time of surgery was 81.37 years (52-97 years, SD: 9.91). 44 patients were woman (62.86%) and 26 patients were men (37.14%). Mean BMI was 22.71(16 - 300, SD 43.86). 2 patients (2.94%) had a BMI greater than 30. At the time of trauma 14 patients (20.59%) were active smokers.
Subtrochanteric fractures were classified according to the Russel-Taylor classification: 55 patients suffered from a type IA (78.57 %), 12 patients type IB (17.15 %) and 3 patients (4.28 %) type IIA. 36 patients (51.43%) required an open reduction.
Group B
Mean age at the time of surgery was 78.9 years (29-99 years, SD: 15.38). 84 patients were woman (67.74 %) and 40 patients were men (32.26%). Mean BMI was 23, 4,17 (17-31, SD 4,17). 8 patients (6.9%) had a BMI greater than 30. At the time of trauma 17 patients (13.79%) were active smokers. Subtrochanteric fractures were classified according to the Russel-Taylor classification: 26 patients suffered from a type IA (20.96 %), 60 patients type IB (48.38 %) and 38 patients (30.65%) type IIA. 48 patients (38.71%) required an open reduction and in 16 patients (12.90%) cerclage were needed in order to maintain an acceptable reduction
Results
Group A
Healing of the fracture was found in 66 patients (94.28%).
Pseudarthrosis was found in 4 cases (5.71%), all treated with closed reduction and no cerclages. 2 of them had a BMI over 25 and the other were active smokers.
Implant failure occurred in 3 cases (4.28%): in one case a new reduction and fixation with a Dynamic Hip Screw Plate (DHS) was needed, in 2 case hip replacement was performed by using a doubled tapered conical stem (Modulus-R stem – Lima corporate)
59 patients (84.29%) returned to social life and at their daily activities prior to the trauma.
Mean VAS at 12 months was 1.55 (1-2, SD 1.28)
Group B
Healing of the fracture was found in 116 patients (94.54%). 2 patients (1.61%), treated with open reduction, suffered from varus consolidation, who did not require surgery.
Pseudarthrosis was found in 8 cases (6.45%), all treated with closed reduction and no cerclages. 6 of them had a BMI over 25 and the other were active smokers. In 2 cases of implant failure required revision surgery was needed and a hip replacement was performed (Modulus-R stem – Lima corporate).
Removal of the nails, upon fracture healing, occurred in 2 patients (1.61%).
102 patients (81.94%) returned to social life and at their daily activities prior to the trauma.
Mean VAS at 12 months was 1.49 (1-2, SD 1.42)
Discussion
Operative management of subtrochanteric fractures intramedullary nails (IM) have become the gold standard.6,7The long medullary nail has a biomechanical advantage over a short nail as it provides better stability due to a longer lever arm and protects the remaining femoral shaft below the fracture site by preventing the appearance of peri-implant fractures. On the other hand, the use of a short nail has several advantages such as shorter operating and fluoroscopic times, lower blood losses and lower costs than the long nail.10
Subtrochanteric fractures usually occur in elderly patients, due to bone frailty, age and comorbidities, or in young people following high-energy traumas, and in both cases, it is important to limit surgical time and limit blood loss during surgery. Considering these factors, the use of a short nail appears to be more advantageous, especially in elderly patients and in young people with multiple traumas.12
We retrospectively compared the two group and we found a high rate of consolidation: 94.28% in group A and 94.54 % in group B. Regarding clinical recovery, the return to social life and to daily activities was similar in the two groups compared (84.29% in group A, 81.94% in group B).
Varus and procurvatum malunion or nonunion are the most common complications of IM fixation due mainly to improper intraoperative anatomical reduction.13–15
We observed 1.61 % of varus deformity and a percentage of pseudarthrosis of 5.71% and 6.45%. Both results are in line with the current literature, which report an incidence of pseudarthrosis and of revision surgery from 2% to 10% and all patients presented a risk factor for non-union.12–16
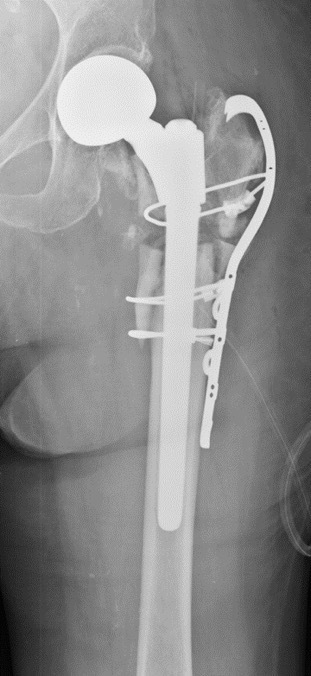
In 4 cases of implant failure hip replacement was needed in order to gain hip stability (Figure 3-4). Modular stems were used in order to obtain a fixation distal as needed and to reconstruct the proximal portion with the length of body. Modular distal-fixation stems ease the intraoperative anatomy reconstruction. A modular double-tapered conical stem was employed in 2 cases of revision of 2 short nail failure, by achieving proximal fit and fill and distal fit in the femoral canal,17 while in other 2 case of failure of long nail a modular tapered conical revision stem18 was needed.
All varus consolidation were found in Russel and Taylor Type IIA fractures. In current literature there is no direct correlation between anatomical classification and malunion.19
In several studies exists a direct correlation between the number of risk factors per patient and the risk of mal-union and non-union.15,16,20,21 Extending the research to other bone segments as well, it appears clearly that there is a direct correlation between smoking habits and pseudo-arthrosis.22,23
About the use of cerclages, they can be a good compromise to obtain and maintain an acceptable reduction by limiting soft tissues invasiveness, but due to their influence on periosteum can lead to pseudoarthrosis.24,25 We employed cerclages in 16 patients, but no one of them had consolidation defects.
Comparison between the two group showed no differences either in terms of radiographic healing or clinical out-come.
Although intramedullary nails are commonly used in subtrochanteric fractures, the indications to use a short rather than a long nail remain unclear and often depend on the surgeon’s habits and preferences. In fact, results reported in literature comparing the two nails do not highlight significant differences.10,26
The limitations of this clinical study, its retrospectivity, and the limited sample size, are common to many other studies concerning this type of fracture due to their low incidence.
Conclusions
The amount of not alignment and the achievement of a good intraoperative reduction, as well as certain risk factors in patient history, correlate with poor clinical and radiographic outcome and with the onset of complications. It is mandatory to consider the characteristics of the patient and to evaluate its risk to develop complications. Obtaining a stable fixation without alignment defects is the key to reach clinical and radiographic healing of subtrochanteric fractures of the femur.
Optimal reduction and fixation, also making use of the use of cerclages, allow in selected patients a high percentage of healing and a good return to social life.
Acknowledgments
None
Author contributions
Author contributions: the authors contributed equally
Conflict of interest
The authors declare that they have no conflict of interest
Funding
None
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.