Introduction
The anterolateral complex (ALC) of the knee has recently regained interest mainly due to the high revision rates in ACLR surgery, despite the recent concepts of anatomical and individualized ACL reconstruction and the vast improvements of fixation methods.1–4 New evidence shows that ACLR revision rates remain unacceptably high, up to 18%, especially in the younger population.5 These failures have a variety of factors, but one of the most concerning is the persisting anterolateral rotatory instability, which may not be fully restored with the current ACLR procedures. It is imperative to search for concomitant pathology in high-grade rotatory knee laxity and revision cases. The pivot shift test following ACLR plays an important role and correlates with functional outcomes. A successful anatomic ACLR is essential before considering an anterolateral extra-articular augmentation procedure.
Research studies have shown that the anterolateral ligament (ALL), a distinct anatomical structure, may play a key role in controlling internal tibial rotation.4,5 Andrade et al., in a recent Systematic Review of MRI studies, comprising of 2,427 knees in 2,388 patients, found that the ALL appeared injured in 11% to 79% of the ACL tears.6 Dhong Won Lee et al., recently reported that ~70% of acute ALL injuries showed poor healing at 1-year follow-up.7 Other studies have shown that the remaining anterolateral rotatory instability after ACLR, is a factor that is associated with poor functional outcomes.8,9 Anterolateral ligament reconstruction and the modified Lemaire technique are two popular procedures for restoring the anterolateral complex (ALC). The indication of Extra-Articular Augmentation (Lateral Extra-Articular Tenodesis [LET] or Anterolateral Ligament [ALL] Reconstruction lately) is well understood, although ALLR has not been thoroughly studied.4,5 Biomechanical studies have reached varied conclusions; however, there is an increase of research that suggests both procedures enhance stability in the surgical treatment of anterolateral instability, whereas ACLR alone is not sufficient in the setting of complex anterolateral injury.10–14
This review aims to present and discuss the most current anatomical, biomechanical, and imaging data, current reconstruction techniques, and the clinical results of ALC reconstruction.
Anatomy and Biomechanics
It has been challenging to distinguish and characterize the anatomical structures of the anterolateral side of the knee joint. Initially, it has been divided into parts and layers. Hughston et al., in 1976 divided the lateral compartment of the knee into three parts: anterior, medium, and posterior.15 Seebacher et al., in 1982 divided the lateral structures of the knee into three layers and described the deepest layer (Layer 3), as splitting into a deep lamina (true knee capsule) and a superficial lamina (ALL), that inserts anterior to the lateral collateral ligament (LCL), and enveloping it.16 Recently, in 2017, it has been proposed that the components of the anterolateral complex (ALC) of the knee joint include (a) the iliotibial band (ITB), (b) the anterolateral ligament (ALL) as a separate ligamentous structure, (c) the anterolateral joint capsule, and (d) the lateral meniscus.17,18
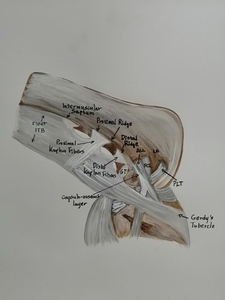
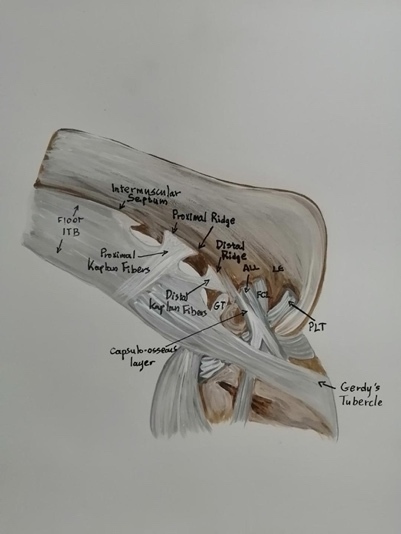
Since 1879, when the French surgeon described the eponymous Segond fracture, numerous anatomic and biomechanical studies with regard to the ALC have been published.4,12,13,19 However, there has been much controversy over the existence or not of the ALL,20–24 the nomenclature,5,14,25–27 the anatomical position,4,14 the stabilizing role4,14,28 and the associated injury with ACL tear.4,14 This anatomical structure has been referred to by a different names. It was not named "anterolateral ligament " until Steven Claes et al. published their study in 2013.14 This term was used by Terry et al., who were the first described the iliotibial tract as the “true anterolateral ligament of the knee”.14,25,29 Hence, in order to clarify the existing confusion, the International ALC Consensus Group Meeting reached a consensus in 2017; the anatomic structures of the anterolateral complex of the knee are: the superficial iliotibial (IT) and the iliopatellar band, the deep IT band incorporating the Kaplan fiber system (supracondylar attachment, proximal and distal) and retrograde (condylar) attachment continuous with the capsulo-osseous layer of the IT band, the ALL and the capsule [Figure 1]. The ALL is considered a capsular structure within Seebacher’s Layer 3 of the anterolateral capsule of the knee. The deep lamina is the true knee capsule and the superficial lamina is the ALL, which has variable gross morphology between individuals with regard to size and thickness, is predominantly attached posterior and proximal to the lateral femoral epicondyle and LCL’s origin, runs superficial to the LCL, attaches to the tibia midway between the anterior border of the fibular head and the posterior border of Gerdy’s Tubercle, and there is an attachment of the ALL to the lateral meniscus.15,17
However, research on ALL is still continuing, and there are still some controversies regarding its existence, in what form and its anatomic point of insertion, especially proximally.17,18
Anatomical studies of the ALL have reported a total length of 30.4-59.0 mm, thicknes of 1.0-2.5 mm and variable widths of 4.0-11.0 mm at the origin, 4.0-8.0 mm at the midpoint, and 11.0-12.0 mm at the insertion.3,30–33
The role of the ALC of the knee in patients suffering from ACL tears is still controversial although many reports suggest that contributes significantly in the rotational stability of the knee.1,5,22 Nevertheless, many studies reported their results without the participation of ITB, which plays a significant role during the pivot-shift testing.34 In a cadaveric study, Junjie Xu et al. reported that the ALC of the knee, played a minor role in controlling anterior translation or pivot shift stability in ACL tear but with the ITB in tension it showed a significant role in restraining internal rotation from 45o to 90o.34 Ahn et al., in a cadaveric biomechanical study investigated ALL behavior during knee flexion-extension, internal-external rotation, anteroposterior translation, and varus-valgus angulation.35 Littlefield et al., in a systematic review of the literature, reported that the ALL plays a secondary stabilizing role to the ACL and helps resisting internal knee rotation and anterior tibial translation.3
Biomechanical studies have reached varied conclusions, suggesting that more research is necessary to reach a conclusion on the biomechanics of ALC of the knee.1,36,37
Imaging
Imaging includes radiographs, magnetic resonance imaging (MRI), and ultrasound (US). Standard knee radiographs including anteroposterior, lateral, Merchant or posteroanterior weight-bearing (Rosenberg view), are usually recommended.5 Saita et al. found that a small lateral femoral condyle and genus recurvartum are associated with greater rotatory instability and should be considered as predictors of a poor outcome from an ACL reconstruction.38
The presence of a Segond fracture is strongly associated with an ALL injury. This fracture presents on conventional radiographs as an elliptic bone fragment (about 10 x 3 mm in size), commonly 3–6 mm lateral tibial plateau, known as the “lateral capsular sign”.39
MRI [Figure 2 (From the authors’ archive)] is the gold standard for assessing the ALC injury.3,40,41 On the coronal and axial images, the ALL is better evaluated.5 In their study, Liebensteiner et al. assessed the ALL and the deep structures of the ITT in healthy knees, and they found that the anterolateral structures of the knee can be determined using MRI.42 Puzzitiello et al., in a systematic review, found that concomitant ALL injuries, in patients with an ACL tear, can be identified on MRI or US with high levels of inter- and intraobserver reliability, and are often associated with a high-grade pivot-shift examination, lateral collateral ligament injury, and lateral femoral condyle and tibial plateau bone bruises.40 However, in patients with chronic ACL injury, determining the extent of ALL injury can be difficult.35
Ultrasound (US) is a valuable imaging tool for ALC injury assessment. However, the number of studies utilizing it is limited and may be more difficult to compare with MRI.3
Classification and Treatment
The grade and the location (tibial or femoral side) of ALL tearing are variable and can impact the decision for surgical intervention.43 Ji Hyun Ahn et al. classified the ALL injury based on MRI findings into four grades (intact ALL, partial tear, nearly complete tear, and complete tear). The intact and partial tears are low-grade injuries and the nearly complete and complete tear are high-grade injuries.44 Ferretti et al. classified ALC injuries in the setting of ACL tears in 4 types [Table 1].6
The combination of ALL and ACL injury has been reported to range from 32% up to 88%.45 Balendra et al. recently reported the presence of an ALC injury in 63% of the patients with ACL tears (39% isolated Kaplan fibre (KF) injuries; 2% isolated ALL injuries and 22% combination of both.45 Dhong Won Lee found that the ALL injury was associated highly with lateral meniscus tears, especially affecting the posterior horn.46 Ji Hyun Ahn et al. found higher incidence in medial meniscus, especially in the posterior horn.44 During clinical assessment, ALC injury is associated with an increased pivot shift, especially in combination with an ACL tear.44,47,48
There is no consensus regarding the best treatment strategy for ALC injury, although there has been significant consensus recently.47 Surgical options include two basic techniques: (a) anterolateral extra-articular tenodesis (AEAPs), with the modified Lemaire being the most preferred technique, and (b) anterolateral complex reconstruction (ALLR).47,49 ALLR is not advised as a routine treatment during ACL reconstruction.50,51 Most surgeons’ indications include young and active patients with rotatory laxity on clinical examination, grade 2–3 pivot-shif testing, generalized ligamentous laxity/genu recurvartum, and imaging findings of acute ALC injury as well as patients who require revision of ACL after a previously well-performed reconstruction when no other reason for failure was identified.44,47
Lateral extra-articular tenodesis (LET)
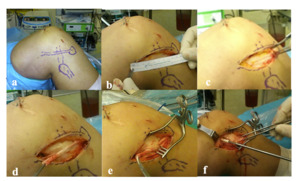
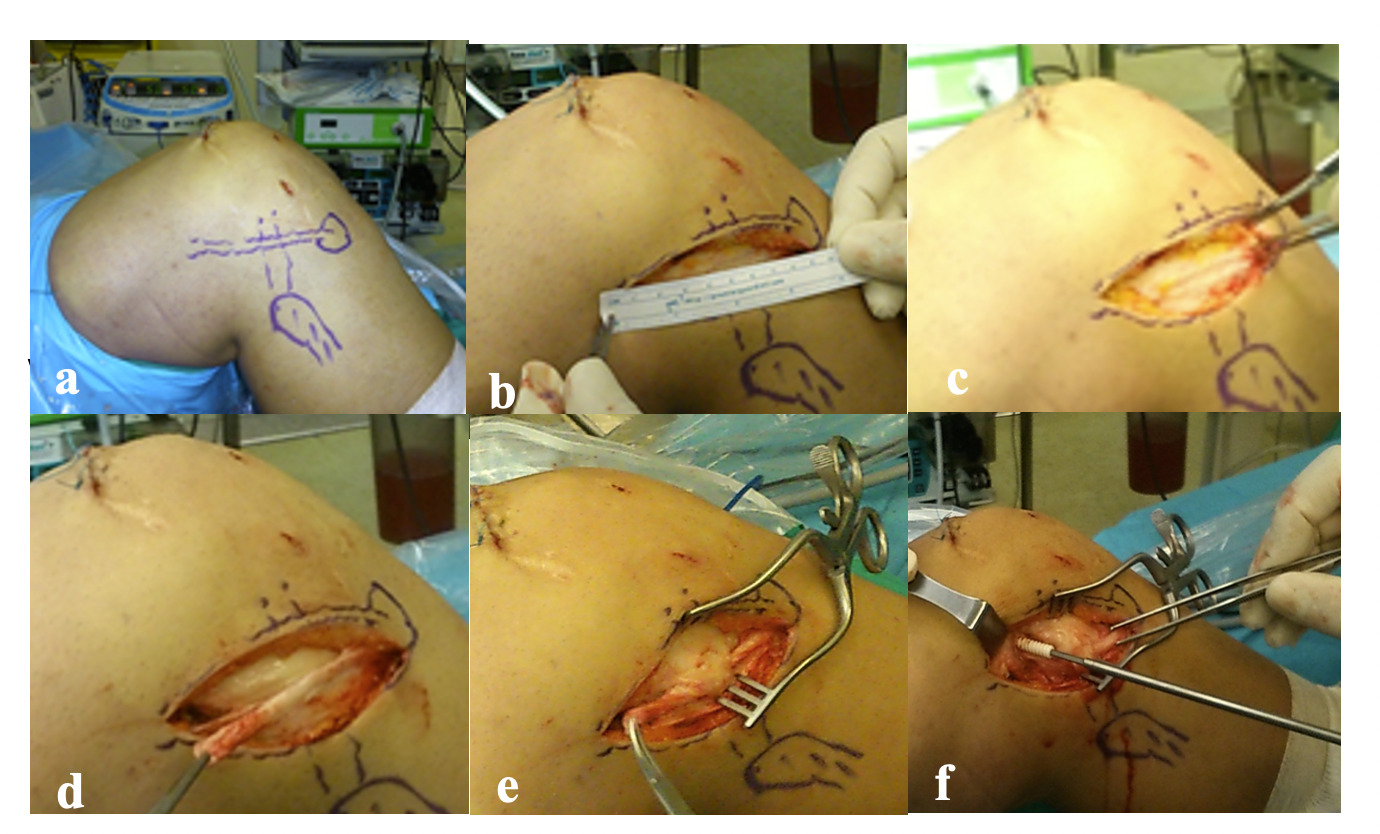
Lemaire since 1967, developed a surgical technique using a strip of ITB, 12 mm wide and 70 to 80 mm long, fixing it posteriorly to the LCL on the femur within a tunnel and distally to the Gerdy tubercle.32 Since then, different modified surgical techniques have been proposed [Figure 3 (From the authors’ archive)], such as those by Dejour et al., Lutz et al., Pavão et al., Jesani et al., and recently Muller et al., and Henri et al.40,52 Other authors have proposed a hamstring graft with Henri et al. having recently published a new surgical technique.52
However, the nonanatomic nature of the LET procedure and the potential over-constraining of the joint can lead to graft over tensioning and degenerative changes in the lateral knee compartment.53 Ferretti et al. and Zaffagnini et al published a long-term study that combined extra- and intra-articular reconstructions, reporting no increased rate of degenerative changes in the lateral compartment.54,55
Anterolateral ligament reconstruction (ALLR)
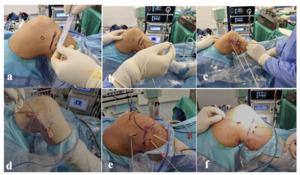
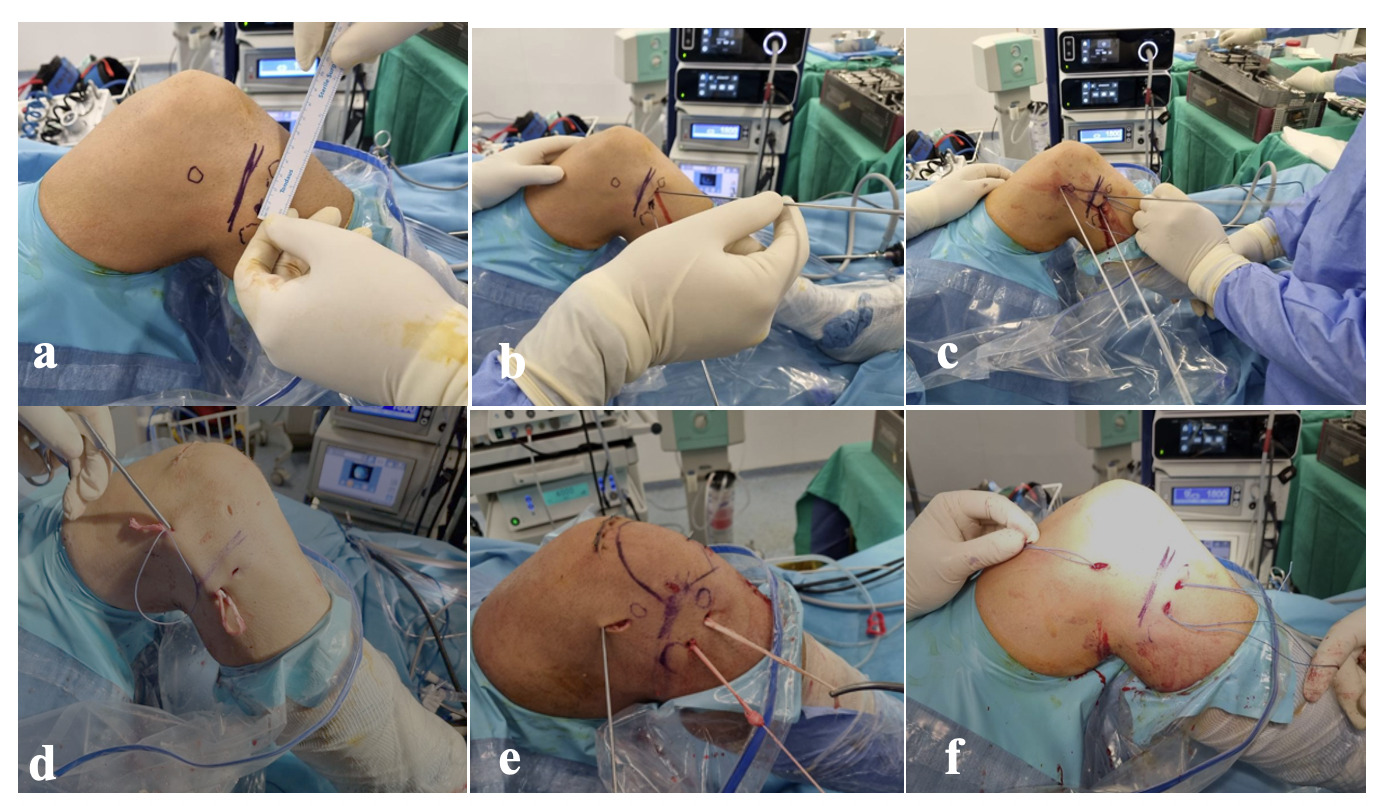
Recently, the renewed interest in the ALC of the knee has led to notable progress in appreciation of anatomy and biomechanics, resulting in the development of new surgical procedures such as the anterolateral ligament reconstruction (ALLR) [Figure 4 (From the authors’ archive)].3,56–59
There is a consensus regarding the ideal positioning of the ALL proximally to the femur and distally to the tibia.12,52 However, there is some disagreement in the literature regarding the precise anatomy of the ALL (in particular, the femoral insertion) and the optimal procedure for reconstruction.56 Some published studies have used an inconsistent surgical technique but the current consensus is in favor of the anatomic ALLR.60–63 This is important to avoid the potential malpositioning or fixation of the graft in an incorrect knee position, which could impact the functional results, render the graft ineffective, or overconstrain the knee.64,65 Based on a cadaveric study, Ahn et al. suggest that during the ALL graft fixation, the knee should be close to full extension.30 The combination of ACLR and ALLR has shown remarkable improvement in clinical results compared with isolated ACLR.66–70
Studies have shown that the most common femoral fixation sites were posterior and proximal to the lateral femoral epicondyle, and for the tibial fixation, the most common sites were between Gerdy’s tubercle and the fibular head.3,70 Regarding the graft’s tension, Kunze et al., in a recent Systematic Review and Meta-Analysis of Randomized Controlled Trials, found that in 9 of 14 studies, the graft was tensioned at 30o.70 The most common grafts used were the gracilis and semitendinosus, and the least used grafts were the quadriceps, Achilles tendon, plantaris, and polyester tape construct.3,70
Outcome
Recent studies have shown that both surgical techniques, ACLR/ALLR and ACLR/LET, are effective procedures to restore ALC stability. In a recent systematic review and meta-analysis, Beckers et al. found a significant reduction in graft ruptures in patients treated with ACLR and lateral augmentation (3%) compared to isolated ACLR (12%) and rotational laxity significantly higher in isolated ACLR (14% vs. ACLR + LA (6%).71 In another recent systematic review, Littlefield et al. reported lower ACL graft failure rates for combined ACLR/ALLR (0.0% - 15.7%) when compared to isolated ACLR patients (7.4% - 21.7%), whereas Kunze et al. reported a failure rate of 2.7%-11.1%, and significant improvement in the IKDC, Lysholm, and Tegner outcome scores postoperatively.3,70 Recent systematic reviews showed that ACLR + ALLR improved patient-reported outcomes at short-term follow-up compared to those who underwent isolated ACLR.3,70 Lee et al., in a comparative study of revision ACLR in combination with ALLR and isolated revision ACLR, found that revision ACLR in combination with ALLR significantly reduced rotational laxity and showed a higher rate of return to the same level of sports activity than revision ACLR alone.72 In a comparative study, Helito et al. found that combined ACL and ALL reconstruction had better rotational stability as evaluated by the pivot-shift test and a lower reconstruction failure rate compared with isolated ACL reconstruction (3.3% vs 21.7%).73 Also, Laboudie et al. found that combined ALL + ACL reconstruction reduced the rate of graft failure and secondary meniscal injury in young athletes when compared to ACL reconstruction alone.74
Recent meta-analysis shows that there is high-level evidence that the LET procedure in addition to ACLR is preferable in terms of functional outcome and graft failure.75 Getgood et al., in a multicenter, prospective, randomized clinical trial comparing a single-bundle, hamstring tendon ACLR with or without LET performed using a strip of iliotibial band, found that the addition of LET to a single-bundle hamstring tendon autograft ACLR in young patients at high risk of failure results in a statistically significant, clinically relevant reduction in graft rupture and persistent rotatory laxity at 2 years after surgery.76 Castoldi et al. in a 19-Year Clinical and Radiological Follow-Up comparative study between ACLR with and without LET found graft failure (29% vs. 13%) and lateral compartment osteoarthritis (59% vs. 22%), correlated with partial meniscectomy.77
Madhan et al in a recent study children and adolescent patients found that 56% of pediatric sports surgeons sometimes perform anterolateral augmentation with primary ACLR and 79% with revision ACLR.78
Another systematic review with the meta-analysis by Na et al.; found that anterolateral ligament reconstruction (ALLR) appeared to be a better option for improving rotational stability compared than extra-articular tenodesis (LET).79
However, more prospective comparative studies are needed to assess if there is a significant difference between two surgical techniques with a view to clinical outcomes.3
Conclusion
Despite some remaining controversies, recent literature shows that there is a consensus regarding the ALL as a ligament and its anatomic location. A combination of anterior cruciate ligament reconstruction (ACLR) and anterolateral ligament reconstruction (ALLR), when ALC injury is associated with an increasing pivot shift, has shown encouraging results in regaining knee function. Further biomechanical studies and long-term clinical studies are necessary.
ACKNOWLEDGEMENT
None
AUTHOR CONTRIBUTIONS
V.A.: Study Design, Literature review, Writing manuscript, Editing manuscript
A.P.: Literature review, Writing manuscript, Editing manuscript, Final manuscript approval
A.K.: Literature review, Writing manuscript, Editing manuscript
Z.K.: Literature review, Editing manuscript, Final manuscript approval
J.L.: Data collection, Editing manuscript, Final manuscript approval
K.K.: Writing manuscript, Editing manuscript, Final manuscript approval
J.G.: Literature review, Writing manuscript, Editing manuscript, Final manuscript approval
DISCLOSURES
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ADDITIONAL INFORMATION
None