INTRODUCTION
Pigmented villonodular synovitis (PVNS) of knee is a rare, histopathologically benign but locally destructive disease. PVNS is a subtype of tenosynovial giant cell tumors that affects synovial membranes, characterized by hemosiderin deposition within synovial-lined anatomic spaces.1,2
Etiology is still debated between a chronic inflammation process or a benign neoplastic lesion. Tenosynovial giant cell tumors can be classified as localized and diffuse: the first form it’s usually extra-articular involving bursae and tendons and it’s characterized by a relatively normal synovial appearance while the diffuse type which is the most common form, is an intra-articular disease characterized by invasion of the contiguous synovium.3
Typically, PVNS is a monoarticular condition that most commonly affects the knee (>75%), while rarely it can involve the hip, wrist, ankle and shoulder. As a matter of fact, the knee joint has the largest reflections of synovial which leads to a higher chance of being involved in synovial disorders. Rarely PVNS can be present a malignant features like metastases.4,5
PVNS occurs predominantly in the early to middle age and has shown to have no gender predilection, but some studies suggest that females are slightly more affected only in the context of localized diseased.6
Onset is insidious with non-specific symptoms like pain, swelling and effusion; but from time to time it could run completely asymptomatic. Thus diagnosis is often delayed for years.
Magnetic resonance (MR) imaging is the most sensitive radiological investigation and it typically shows a mass-like synovial proliferation with roughly lobulated margins. Soft masses with low signal intensity, due to paramagnetic effect of hemosiderin deposition, and “blooming artifact” appear to be pathognomonic of PVNS.1,7,8 High signal may be present in STIR and in T2-weighted images if there are joint fluid or inflamed synovium. Bone erosion and subchondral cysts may be seen and well defined with Computer Tomography (CT). However, histopathologic examination of synovial biopsy remains the gold standard to confirm the diagnosis.
If not treated PVNS can cause degeneration of the joint and osteoarthritis.
In order to treat symptoms and prevent joint degeneration, choice of treatment for PVNS often leads to surgical excision.
We present a case series of 20 patients consequently treated for PVNS of the knee focusing on diagnostic approach, surgical techniques adopted based on disease form and localization, and on the relative outcomes.
MATERIALS AND METHODS
This single-center retrospective study was approved by our local ethics committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.9
Our study consisted of a retrospective analysis of 20 consecutive patients who underwent open synovectomy due to PVNS of the knee between July 2016 and July 2020. They were 7 males and 13 females, with a mean age of 47.2 (15- 80) years. In 2 cases the diagnosis of PVNS was incidental, while the remaining 18 had complained knee pain, stiffness or swelling that brought them to our attention. On average, diagnosis was made 6.8 months (0-25) after the onset of the symptoms. Each patient underwent pre-operative knee MRI, which was used for both diagnosis and surgical planning; the mean size of the neoplasm object of resection was 35.7mm (18 – 61). Pre-operative functionality was assessed using the MSTS Score for lower limbs, whose mean value was 21.7 (16-30).
In light of the mass’ localization, an anterior surgical approach was performed in 15 cases, while a posterior surgical approach was performed in 4 cases. One patient, due to the size of the huge mass that had to be removed, was treated in two separate stages, the first with posterior approach and then anterior within 40 days from each other. The mean surgical time was 74.5 minutes: 93 (75 – 130) minutes for those who underwent posterior approaches and 68.7 (30 - 130) minutes for the anterior ones.
For the anterior approach the patient was in supine position with a tourniquet inflated at the thigh; the surgeon performed a midline longitudinal skin incision and afterwards a medial or lateral parapatellar arthrotomy, depending on the case.
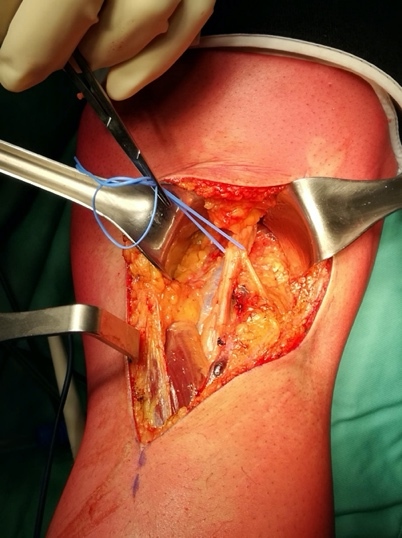
For the posterior approach the patient was in prone position with a tourniquet inflated at the thigh; a s-shaped incision was made starting from the tendon of the biceps femoris then across the popliteal fossa end the medial head of the gastrocnemius (fig.1); the neurovascular bundle was identified and gently moved in order to explore all the anatomic spaces (fig. 2-3).
In both cases a closed suction drain was placed and the wound was closed in layers.
None of our patients underwent neo-adjuvant or adjuvant systemic treatment nor radiant therapy.
Postoperative follow-up consisted of serial office visits, clinical evaluations and post-operative MRIs. All the complications with grade II or higher according to the Clavien – Dindo Classification were reported.10 Patients’ global post-operative performances were evaluated using the MSTS score. In parallel, the OKS was used to assess functional results of both the injured and the contralateral knee.
Statistical analysis were performed using Stata SE 13 (StataCorp LLC, College Station, TX). Correlation between tumor size and functionality, assessed both before and after surgery using MSTS and OKS scores, was calculated using the Pearson correlation test. The same test was also used to evaluate the link between pre-operative dimension itself and the differential among the scores of the two limbs of the same patient. For each couple of variables, we obtained a correlation value (“r” value) and combined this latter and the number of cases under examination (20) to assess its significance level (“p” value). Statistical significance was set at 0.05 for all endpoints.
RESULTS
Clinical and functional results of our population are summarized in Table 1. The mean follow-up was 27.9 (56 – 8) months. Only 1 patient (5%) suffered local complications of grade II or higher according to the Clavien – Dindo classification: a post-operative hematoma treated successfully with ultrasound-guided percutaneous drainage. 3 cases (15%) had a local recurrence of the disease, all diffuse form and respectively 3, 9 and 18 months after surgery (Fig. 4).
At the latest follow-up, our patients’ mean MSTS score was 26.4 (30-18): 27.4 (19-30) for those treated with posterior approach and 26.1 (18 – 30) for the anterior ones. On average, post-operative values were 4.7 higher than the one recorded before the intervention. In 18 cases (90%) the post-operative score was increased compared to the pre-operative one, one case (5%) maintained the same score and one last case (5%) saw a slight worsening of her lower limb functionality. The mean Oxford Knee Score of the injured knees was 41 (19-48), 40.3 for the subpopulation treated with anterior approach and 43.2 for those who were treated posteriorly. The OKS for contralateral knees was 44.4, being good or excellent in all our 20 cases and exceeding the mean value of the injured knees by 3.4. In 13 cases (65%) the injured knee had a lower score compared to the healthy one, in 6 cases (30%) the scores were equivalent, while in one single patient (5%) the treated knee was more performant than the contralateral one.
Statistical analysis defined not only a negative correlation between tumor size and pre-operative MSTS score (Pearson correlation coefficient r=-0.474; p=0.035), but also an even more marked negative correlation between tumor size and the post-operative knee functionality, assessed by using the MSTS score (r=-0.651; p=0.002) and the OKS (r=-0.659; p=0.002). Our data also seem to suggest a negative correlation between tumor size and the spread between the post-operative functionalities of the injured and the contralateral knee according to the OKS (r=-0.313). However, the size of our population was not big enough to provide any statistically significant evidence in this regard (p=0.179).
DISCUSSION
PVNS of the knee is a local aggressive condition causing loss of motion, pain and if not excised, bone erosion and osteoarthritis. Several options of treatment have been described, however surgical excision is currently considered as a gold standard. Depending on the type of PVNS (i.e. local or diffuse) surgical excision is usually marginal for the nodular variant and intralesional for the diffused form, removing all macroscopic visible mass. The difficulty to achieve marginal excision, especially for diffuse form, effects a high recurrence rate of PVNS, even when properly treated.
The surgical approach consists in partial or total synovectomy, where total includes synovectomy of the posterior compartment; both have been described for managing this condition, with varying results. Technically speaking the excision can be performed as arthroscopic or open synovectomy, being both valuable options: the first can be used for localized and intra-articular forms, the second is the best choice for extra-articular or diffuse forms or in case of relapse.11–13 Arthroscopic synovectomy requires a very careful evaluation of pre-operative MRI to detect if the disease involves areas not usually accessed during arthroscopy: the access to the posterior knee can be technically demanding and risky for the proximity to important nerves and blood vessels. Some authors have described the combination of different arthroscopic portals in order to explore almost the whole joint, however we believe that arthroscopic treatment of PVNS in difficult areas should be performed by trained and skilled surgeons.14 Actually, omitting compartments difficult to explore arthroscopically can dramatically change the recurrence rate in diffuse PVNS. On the other hand arthroscopic excision in case of nodular forms of PVNS gives good results with a low recurrence rate.15 Open synovectomy certainly allows for better exposure than arthroscopic approach, however some authors report longer hospitalization, longer rehabilitation period and the risk of postoperative stiffness of the knee.16,17 In our casuistry we did not report any case of arthroscopic excision since all patients had diffuse PVNS, so we performed exclusively open synovectomy; however this did not seem to affect functional recovery, since we reported a post-operative worsening of limb functionality only in 5% of cases. Open synovectomy must be considered also in case of spreading of the disease with the detection of extra-articular foci at MRI.13,17
When a total open synovectomy is planned, it is performed with two separate incisions in order to explore all knee anatomic spaces. The two approaches can be simultaneous in one single procedure or staged in in two different times. Actually both alternatives seem to give good results in terms of recurrence and disease control.17,18 However, a staged approach can lead to easier rehabilitation, with better functional recovery, and allows to shorten surgical times and their potential complication.19 When a double access was necessary, we preferred staged procedure, obtaining both good control of disease and functional recovery.
Partial synovectomy has been associated to high rate of recurrence ranging from 50% to 75%.12 Other studies report a recurrence rate ranging from 14 to 55% even after a total synovectomy.20 We treated all of our patients with open synovectomy, partial or total depending on the cases and we reported a percentage of 15% of recurrence.
Currently also some forms of adjuvant therapy such as radiosynovectomy via intra-articular injection or external beam radiation have been described.13,21,22 These therapies seems to be effective but they do not give any advantage in terms of recurrence over surgery alone; that is why most authors believe the key to preventing recurrence is meticulous surgical synovectomy. Moreover, considering the potential risks of these procedures, especially skin necrosis, wound dehiscence, pathologic fractures and secondary malignancy, it is best to reserve adjuvant therapies to recurrent diffuse forms of PVNS.13,23
Our casuistry consisted in a series of patients with knee diffused PVNS treated all with open synovectomy with anterior or posterior approach, except for one case who had both approaches. The recurrence rates are consistent with literature results, even if the short follow up can be considered as a limit. As predictable, we found a negative correlation between size and spread of disease and functional recovery, however also in this case the exiguous number of patients was a limit in order to prove statistical significancy.
CONCLUSION
In our experience, a thorough study of preoperative MRI and an optimal surgical exposure were the key to obtain good results; the knowledge of anatomy and the awareness in performing all surgical approaches to the knee allows for optimal excision reducing thus the recurrence rate in the short-middle time. Moreover we believe that staging the different approaches could be helpful in obtaining a good recovery, especially in complicated patients. Finally, in very challenging cases a multidisciplinary approach, including an experienced surgeon, an oncologist and a radiation specialist is mandatory.
Authors’ contributions
Fabio Cosseddu - design of the study, drafting the manuscript and interpretation of data;
Edoardo Ipponi – conception of the study and statistical analysis;
Alfio Damiano Ruinato – data collection and drafting of intro;
Sheila Shytaj – drafting of manuscript and interpretation of data; English revision;
Rodolfo Capanna – critically revision of the manuscript for important intellectual content;
Lorenzo Andreani – critically revision of content and final approval of definitive version;
Conflict of interest
All Authors that have contributed to this work declare no have any conflict of interest or funding.