Introduction
The tarsometatarsal (TMT) joint in the midfoot, commonly referred to as the Lisfranc joint, is named after the famous French gynecologist, Jacques Lisfranc de Saint-Martin, who trained under Guillaume Dupuytren and served as a field surgeon for Napoleon’s wartime army.1 In 1815, he was the first to describe the Lisfranc injury and developed a midfoot amputation at the TMT joint to treat frostbitten and gangrenous feet that resulted from this injury.2,3 In one particular case, Jacques Lisfranc amputated a gangrenous foot that resulted in a Lisfranc injury after a soldier’s foot was caught in a stirrup.4,5
The Lisfranc joint complex consists of three articulations including tarsometatarsal, intermetatarsal, and intertarsal articulations, which provide fundamental stability from the keystone arrangement of the bones.6 The TMT joint is composed of three layers of ligamentous support.7 From strongest to weakest, the interosseous layer, which includes the Lisfranc ligament, provides the most support followed by the plantar layer and then the dorsal layer.8 Several ligaments further reinforce this joint complex and limit motion including the Lisfranc ligament, plantar tarsometatarsal ligaments, dorsal tarsometatarsal ligaments, and intermetatarsal ligaments.9 The Lisfranc ligament, also known as the oblique interosseous ligament, is the strongest stabilizer of the tarsal metatarsal joint complex.10 It extends from the plantar lateral aspect of the medial cuneiform to the plantar medial aspect of the base of the second metatarsal.11
When Lisfranc injuries occur, they can be bony, ligamentous, or a combination of the two. Injuries to this joint are two to four times more likely in males and occur at a commonly reported incidence of 1 per 55,000 people while accounting for 0.2% of all fractures.1,3 It is important to note that Lisfranc injuries are often underdiagnosed with a 2020 study by Stødle et al. reporting the incidence of these injuries to be as high as 14/100,000 person-years.12 Lisfranc injuries are commonly classified under the Hardcastle and Myerson classification system, which divides the injuries into Type A, B1, B2, C1, and C2.13 Type A injuries encompass dislocation of all metatarsals in one direction (homolateral). Type B injuries involve partial dislocation of either the medial (B1) or lateral column (B2). Type C comprises a divergent dislocation, which is either partial (C1) or complete (C2).3
Lisfranc injuries can be caused by direct or indirect forces. Direct mechanisms generally involve a high-energy crush injury causing displacement of the metatarsal bases. Indirect mechanisms involve rotational forces applied to the forefoot or axial loading of a hyper-plantarflexed foot.5 While examining the mechanisms of Lisfranc injuries, Stødle et al. reported 21% were sports-related and 31% were due to high-energy mechanisms including motor vehicle collisions, falls from greater than 3 feet, and crush injuries. The single most common documented mechanism of injury was a fall from a standing height with a twisting injury to the foot.12 With several treatment options available, management of Lisfranc injuries is still controversial, especially when the injury involves only ligamentous structures.14
In this unique case, the Lisfranc ligament was directly transected by a sharp object puncturing through the plantar surface of the patient’s foot such that there was little to no translational force in this disruption. With this mechanism of injury, surgical transection of the Lisfranc ligament was mimicked, thus resulting in a rare injury type.
Case Presentation
Initial Care
A 23-year-old male with no significant past medical history presented to the emergency department with a large metal spike through his right midfoot measuring approximately 1.5 cm in diameter by 20 cm in length. As the patient was working on a construction site, he was using his feet to crush objects while wearing rubber-sole tennis shoes. When he stepped on a large roof turbine fan, the peripheral blades collapsed, which resulted in his right foot landing on the metal axle in the center and impaling the foot. On arrival at the emergency department, the roof vent was attached with the metal axle penetrating through his shoe sole and the bottom of his foot. The emergency department staff disassembled and removed the portions of the vent that were easily accessible. The patient’s chief complaint was significant pain in the foot, and he received cefazolin for skin flora coverage, penicillin for spore-forming bacteria coverage, ciprofloxacin for Pseudomonas coverage, and a tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in the emergency department.15,16
On physical exam, a large metal spike penetrated from the plantar midfoot through the subcutaneous tissue and extended to the dorsal aspect of the midfoot with notable skin tenting (Figure 1). The patient had intact motor function and sensation to a light touch of the right lower extremity with a dopplerable triphasic dorsalis pedis pulse. Initial radiographs were obtained to characterize the injury (Figure 2). After discussing the risks and benefits of all treatment options, the patient elected to proceed with staged procedures due to the high risk of infection from the open wound and the possibility of a fracture/dislocation injury associated with the impalement of the midfoot.
Surgical Care
Procedure 1
The patient was taken to the operating room and general endotracheal anesthesia was induced without complications. The right lower extremity was cleaned with isopropyl alcohol before placing an impervious nonsterile drape about the thigh. A standard 2g of intravenous cefazolin was then administered. After cutting off a portion of the shoe and sock, these objects were slid distally away from the plantar aspect of the foot. Povidone-iodine was poured over the entirety of the right foot. Axial traction perpendicular to the planter surface of the foot was then applied to pull the metal spike away from the plantar surface while grasping the forefoot and midfoot for countertraction. The large foreign body left a 1 cm x 1 cm circular void on the plantar surface of the foot, however, there was no sign of fracture after removal. Fluoroscopic imaging was used to confirm all remnants of the foreign body object were removed (Figure 3).
The right lower extremity was prepped and draped in a standard fashion. The penetrating wound was explored and debrided to clean all open sites of any retained particles. A 4 cm incision was created over the dorsal surface of the foot between the first and second rays where the metal spike had previously protruded and was tenting the skin. Dissection was performed on the 2nd and 3rd TMT joints. Obvious traumatic rupture of the dorsal capsular tissue at the 2nd and 3rd TMT joints was noted along with a divergent pattern of lateral subluxation at the 1st and 2nd metatarsal bases where the impalement device had previously penetrated (Figure 4). After excisional debridement of devitalized tissue, healthy bleeding tissue was exposed, and the area was thoroughly irrigated. The antibiotic powder was directly placed into the depths of these wounds.
The TMT joint was manipulated back into a reduced position from a lateral subluxation, and this was confirmed on fluoroscopy. Due to obvious contamination from the open injury, ORIF was not felt to be indicated at that moment. Therefore, the wounds were closed and sterilely dressed. A well-padded short-leg posterior slab splint was placed. The patient was placed on non-weight-bearing precautions to the right lower extremity. Aspirin 325 mg daily was initiated for deep vein thrombosis prophylaxis. Postoperative radiographs were obtained to confirm the alignment and reduction of the midfoot (Figure 5). The patient was then admitted to the hospital overnight for pain control and continuation of intravenous antibiotic therapy. Upon discharge, the patient was given a prescription of oral cephalexin 500 mg four times daily, aspirin 325 mg daily, pain medication, and an appointment for a 1-week follow-up for a wound check.
At the 1-week follow-up, the dorsal and plantar wounds were well-healing with minimal swelling and no evidence of infection. The patient was then scheduled for definitive surgery 2 weeks later and advised to stop aspirin the day before his second surgery.
Procedure 2
The patient was given a preoperative regional block before being taken to the operating room and general endotracheal anesthesia was induced without complications. The patient was positioned, prepped, and draped in the same manner as the initial procedure and given 2 g of intravenous cefazolin for surgical prophylaxis.
After reopening the dorsal wound, the subcutaneous plane was recreated and irrigated. Dissection to the first web space between the first and second rays provided exposure to the midfoot joint. Upon assessment, there was evidence of complete avulsion of the dorsal capsular ligament over the second and third TMT joint with obvious instability as noted in the index procedure.
Surgical fixation was initiated at the intertarsal joint between the medial and intermediate cuneiforms to reduce the tarsal bone dislocation. Using fluoroscopic imaging, a lateral image was obtained to identify the proximal mid-portion of the medial cuneiform as the starting point. On anteroposterior fluoroscopic imaging, drill holes were created in the intercuneiform joint between the medial and intermediate cuneiforms before placing a Synthes 2.7 mm x 46 mm fully-threaded cortex screw (DePuy Synthes, Raynham, MA, USA) by lag technique to achieve compression fixation.
When addressing the 2nd and 3rd TMT joint, the 2nd TMT joint was initially clamped into position under direct visualization before placing a small Kirschner wire (K-wire) across the joint to maintain the reduction. A drill guide for continuous compression implants was centered in position over the second TMT joint with drill holes then into the base of the second metatarsal and into the central portion of the intermediate cuneiform. Two bi-cortical drill holes were created in accordance with the guide. An 18 mm BME ELITE™ Continuous Compression Implants (BioMedical Enterprises ELITE; DePuy Synthes, Raynham, MA, USA) was then impacted into the drill holes to achieve compression. A lateral counter incision was created with the appropriate skin bridge approximately 2.5 cm in length overlying the 3rd and 4th webspace at the level of the TMT joints. After dissection, the 3rd TMT joint was reduced and temporarily fixed with a K-wire under direct visualization. The drill guide was then introduced over the bone center at the 3rd TMT joint. Two bi-cortical drill holes were created in accordance with the guide, and another 18 mm BME ELITE™ Continuous Compression Implants (BioMedical Enterprises ELITE; DePuy Synthes, Raynham, MA, USA) were then impacted into the drill holes to achieve compression. Fluoroscopic imaging confirmed anatomic reduction and satisfactory implant positioning with no instability when the midfoot was stressed (Figure 6). Then, the incision sites were thoroughly irrigated, closed, and sterilely dressed.
Postoperative Care
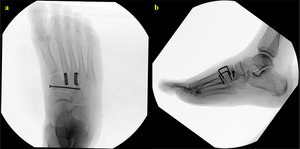
Postoperatively, the patient was placed on non-weight-bearing precautions to the right lower extremity for 6 to 8 weeks and early range of motion of the toes and foot was encouraged. Aspirin 325 mg daily was continued for deep vein thrombosis prophylaxis for two weeks. At the 6-week follow-up visit, the patient had minimal pain with well-healed incisions. There was no evidence of wound complications or infection. Postoperative radiographs were obtained to confirm alignment and reduction of the midfoot, which were well maintained (Figure 7). After progressing the right lower extremity to a partial weight-bearing status in a Controlled Ankle Motion (CAM) boot, the patient started a rehabilitation program with physical therapy.
Discussion
Penetrative Lisfranc injuries are rare, with only one other case report involving a brake pedal reported in the literature.17 However, penetrating foreign body injuries to the foot are relatively common, compromising approximately 40-50% of patients presenting with a foreign body in the extremities.18,19 Metal, glass, wood, and plastic are all materials that may be involved with needles being the most common object.18,19 When foot injuries involve penetration by foreign objects, plain radiographs should be obtained and will reliably reveal metal and most glass objects. Ultrasound, computerized tomography (CT), or magnetic resonance imaging (MRI) may also be useful to help detect radiolucent foreign bodies. Easily accessible foreign bodies can often be removed in the emergency department under local anesthesia, whereas deep objects may require careful surgical exploration in the operating room. With rates between 3-12% for those seeking treatment, infection has been reported as the most common complication from these injuries.19,20 Typically, Staphylococcus aureus is the most commonly isolated organism from cultures.19,21 In a case series investigating nail puncture wounds through a rubber-soled shoe, out of the 24 positive wound cultures identified, 12 grew Staphylococcus aureus (11 methicillin-sensitive Staphylococcus aureus (MSSA) and 1 methicillin-resistant Staphylococcus aureus (MRSA)) while only 3 grew Pseudomonas aeruginosa.21 Therefore, antibiotic administration should provide coverage for both gram-positive (Staphylococcus aureus) and gram-negative (Pseudomonas aeruginosa) organisms. Additionally, it may be useful to consider the treatment algorithm proposed by Rubin et al. to reduce the risk of infection after a puncture injury to the foot, which involves prophylactic oral antibiotics for patients not indicated for surgical management, postoperative oral antibiotics for patients undergoing surgical nail removal, and possible admission for IV antibiotics for high-risk patients and those presenting with recurrent infections or treatment failures.21
Lisfranc injuries can be treated in several ways depending on the severity and type of injury. Current treatment options include nonoperative management with cast immobilization and operative treatment with closed reduction and percutaneous pinning (CRPP), open reduction internal fixation (ORIF), and primary arthrodesis.22 Cast immobilization is generally reserved for sprains in which weight-bearing x-rays and stress views do not demonstrate displacement.1 Nonoperative treatment has been reported to yield satisfactory results for non-displaced injuries, even in athletes.23 For unstable Lisfranc injuries and those with displacement (2-5 mm), operative management has been reported to be the standard of care due to poor outcomes associated with nonoperative treatment.22 Closed reduction and percutaneous pinning with K-wires is another surgical option. However, screw fixation has been documented to be more rigid and stable in biomechanical studies and only the lateral column has been reported to be satisfactorily stabilized with K-wire pinning.22,24
Specific strategies for operative fixation of Lisfranc injuries have been proposed including open reduction internal fixation with dorsal plates, transarticular screws, surgical staples, suture buttons, k-wires, and primary arthrodesis. While the optimal surgical option is still debated, the two main open surgical treatment options are ORIF and primary arthrodesis. The results of studies comparing the two methods have yielded mixed results in terms of which option produces more favorable outcomes. A prospective randomized control trial by Henning et al. demonstrated no difference in outcome scores between ORIF and arthrodesis, however, there was an increase in the rate of subsequent procedures reported in the ORIF group with hardware removal cited as the primary reason for reoperations.25 A meta-analysis by Smith et al. noted similar findings based on the available literature but documented one of their limitations as a lack of large prospective comparative trials due to the low incidence of Lisfranc injuries.26 In another study, Barnds et al. concluded primary arthrodesis to be more costly and associated with an increased rate of complications compared to ORIF.27 Contrary to Barnds et al., other studies have determined primary arthrodesis to be favorable compared to ORIF with the arthrodesis group having higher American Orthopedic Foot and Ankle (AOFAS) scores, a better rate of returning to work-related duties, shorter surgical times, and fewer complications.28,29 Regardless of the surgical treatment option, the precise anatomic reduction has been well documented to be the most important factor in achieving favorable outcomes following surgery.30
Hardware removal is commonly performed in the months following ORIF for Lisfranc injuries.31 Indications for hardware removal include painful hardware, hardware loosening, infection, hardware breakage or preemptive removal to allow for joint motion, and avoidance of hardware failure complications.31,32 In a 2018 study comparing Lisfranc injury management, Barnds et al. determined patients with ORIF had a significantly higher rate of hardware removal (43.6% vs. 18.4%, p < 0.001) than patients with a primary arthrodesis.27 Additionally, Henning et al. reported hardware removal as standard protocol for all patients with Lisfranc injuries treated with ORIF.25 Kellam et al. further demonstrated that hardware removal was associated with an overall complication rate of 9.6% including unexpected reoperations, readmissions, wound healing delay, infection, continuing pain, nerve injury, and fracture.33 However, this study included all types of hardware removal and was not specific to hardware removal after ORIF for Lisfranc injuries. In another study investigating Lisfranc removal of hardware, the rate of deep peroneal nerve injury rose from 11% after the initial fixation surgery to 23% after the removal of hardware.34 Removal of hardware for Lisfranc is not without risks of possible loss of reduction, secondary osteoarthritis, and deformity.35 Other disadvantages include greater anesthesia time, increased time off work, delay in rehabilitation, and while there is a theoretical benefit of optimizing motion and midfoot biomechanics, these benefits remain unproven.36 Each of these factors are important to consider when choosing between ORIF and primary arthrodesis.
The controversy surrounding the optimal fixation method still remains in part due to the heterogeneous nature of Lisfranc injuries, which present with a wide range of severities, varying instability patterns, and different levels of intraarticular damage. In a 2019 study examining implant fixation stability following a simulated Lisfranc injury, Ho et al. demonstrated a novel Lisfranc plate to have comparable stability to transarticular screws in terms of motion across the Lisfranc joint.37 Additionally, a 2020 study by Scofield et al. reported patients treated with a Lisfranc screw in addition to joint-preserving dorsal fixation using staples or plates had comparable outcomes scores to patients treated with transarticular screws.38 Although different construct types can be used, direct visualization is necessary to help identify instability patterns and assist with obtaining a stable anatomic reduction to improve patient outcomes.6,39
In this particular case, surgical management was chosen for our patient due to the unstable nature of the ligamentous Lisfranc injury, which would result in long-term disability if treated nonoperatively.40 Although similar functional outcomes have been reported, ORIF was selected due to concerns of forefoot stiffness, loss of metatarsal arch, development of pseudoarthrosis, difficulty wearing shoes, and sympathetic dystrophy associated with primary arthrodesis.41 Additionally, when compared to primary arthrodesis, ORIF is a cartilage-sparing procedure that preserves the joint, and our active, healthy, 23-year-old construction worker did not have extensive articular cartilage damage upon injury assessment during the index procedure or evidence of pre-existing midfoot arthritis, which would have directed us to perform a primary arthrodesis as a more favorable option.6,38 Interosseous transarticular solid-screw fixation across the intercuneiform joint was utilized to rigidly hold reduction to allow the ligaments to heal.42 A Lisfranc screw is routinely placed for the reduction and stabilization of diastases between the medial cuneiform and the base of the second metatarsal after a ligamentous Lisfranc injury.43 However, when all involved TMT and intertarsal joints were stressed intraoperatively for our patient, instability was noted in the 2nd and 3rd TMT joints as well as both intercuneiform joints but there was no evidence of instability or disruption of dorsal structures at the 1st TMT joint. Therefore, fixation across the 1st TMT joint was not felt to be warranted. Although extraarticular dorsal plate fixation was an option to address the 2nd and 3rd TMT joint, the 2-legged nitinol compression staples were the surgeon’s preference and were specifically selected for their ease of use, low profile, and maximization of joint stability after reduction.44,45 The articular surfaces at the TMT joints were intact and therefore these joints were preserved. A single screw was used across the intercuneiform joints as this provided stable fixation with minimal additional soft tissue disruption. By stabilizing the 2nd and 3rd TMT joints as well as the intercuneiform joints, the medial column was reduced to the middle column, and a stable construct was achieved. This obviated the need for an additional screw across the medial cuneiform to the base of the 2nd metatarsal. In addition, due to the skin tenting caused by the foreign body object, the tenuous dorsal soft tissue of the midfoot was noted during the initial procedure after opening and exploring the dorsal capsular tissue space.46 Therefore, prominent hardware such as an extraarticular dorsal plate was avoided in the second procedure to maintain the integrity of the thin soft tissue of the dorsal foot and prevent the possibility of wound dehiscence due to skin breakdown.47,48
It is interesting to note that there is a lack of consensus amongst orthopaedic trauma surgeons and foot and ankle specialists regarding the terminology to describe primary arthrodesis and ORIF of the foot. Traditionally, arthrodesis has been reserved to describe the removal of cartilage and fusion of a joint while ORIF has been used to encompass all other fixation methods utilizing plates and screws across joints. However, in situations where the cartilage is preserved and temporary stabilization of the joint is obtained through fixation, there is ambiguity in describing this as either ORIF or primary arthrodesis. Although cartilage has not been removed, some surgeons may view the joint as fused due to reduced motion until the hardware is removed while others may regard arthrodesis as a misnomer for this type of procedure. Therefore, we propose the use of the new term “open reduction internal stabilization (ORIS)” to describe the stabilization of a joint without removing cartilage. This nomenclature may also be helpful in clearly delineating surgeries in other joints where cartilage is preserved and hardware is placed including sacroiliac joint screw fixation.
Conclusion
Mimicking a surgical transection, a direct Lisfranc ligament injury via a sharp object puncture through the plantar surface of the midfoot is a rare condition, which may result in long-term disability if missed or untreated. The initial surgery for our patient focused on removal of the foreign body object, irrigation and debridement of the wound site, injury assessment, and closed treatment of the injury site after reduction. Definitive treatment of the dislocated TMT joints associated with the Lisfranc ligament injury entailed the utilization of a cortical compression screw lagged by technique and staple fixation. This case report highlighted the difficulties of removing a large foreign body object, the importance of planning staged procedures, and the intraoperative techniques used to obtain an optimal outcome.
Acknowledgment
None
Author Contributions
W.S.: Study design, Editing manuscript, Final manuscript approval
A.P.: Chart review, Image formatting, Writing manuscript, Editing manuscript
M.W.: Literature review, Writing manuscript, Editing manuscript
N.G.: Literature review, Chart review, Writing manuscript
W.S.: Study design, Editing manuscript, Final manuscript approval
Disclosures
All conflicts of interest have been identified, and there has been no significant financial support or funding for this work that could have influenced its outcome.
Additional information
IRB exemption was given by Tulane University Human Research Protection Office for Study Reference#: 2022-463

_a_top_view_and_(b)_a_s.jpeg)
_anteroposterior_(ap)_and_(b)_lateral_of_the_right_foot_.tiff)

_forceps_pointing.jpeg)
_ap__(b)_oblique__and_(c)_lateral_of_the_ri.jpeg)
_ap__(b)_oblique__and_(c)_lat.jpeg)
_a_top_view_and_(b)_a_s.jpeg)
_anteroposterior_(ap)_and_(b)_lateral_of_the_right_foot_.tiff)

_forceps_pointing.jpeg)
_ap__(b)_oblique__and_(c)_lateral_of_the_ri.jpeg)

_ap__(b)_oblique__and_(c)_lat.jpeg)