1. Introduction
Total Hip Arthroplasty (THA) is considered the most effective treatment for end-stage degenerative hip osteoarthritis (OA), providing pain relief, restoring joint function, and improving patient’s quality of life.1 For the successful outcome of the procedure, it is important to maximize the impingement-free range of motion, recreate appropriate offset, and equalize limb length discrepancies.2 Various approaches may be performed during surgery and the most commonly used include the posterior, posterolateral, direct anterior, anterolateral, and direct lateral approaches. Depending on the position of the patient, anterior approaches can be performed in either the supine (Anterior approach in supine position and Anterolateral supine approach) or lateral decubitus (Direct anterior approach in lateral decubitus and Anterolateral lateral approach) as well as direct lateral approaches, while posterior approaches require the patient to stay in lateral decubitus. In lateral decubitus the patient is placed with the hip to operate on the top. Adequate padding is then required with double support, on the front for the superior iliac spine and back for the sacrum, to keep the patient’s position and sustain the bony pelvis (Figure A and B). In the supine position the patient is placed supine on the table, with an arch to support the ipsilateral arm and a table attachment at the contralateral hip to stabilize the patient during surgery (Figure C). All of the approaches have a series of advantage and disadvantage: direct anterior approach preserves the integrity of the muscular tissue and posterior capsule, resulting in less soft tissue damage and reducing the risk of dislocation,3 but has a higher risk of lateral femoral cutaneous nerve injury 4 and it is also associated with a series of complications, such as femoral and trochanteric fractures, femoral and acetabular perforation and dislocation if performed in the supine position, while may lead to a cup malposition if performed in lateral decubitus.5 Anterolateral approach provides better visualization of the acetabulum, allowing to preserve the integrity of the posterior capsular structures and short external rotators, and a low dislocation rate, but it may also lead to an increased incidence of abductor dysfunction when performed in supine position.6 The direct lateral approach provides extensive exposure to the femur and has a low dislocation rate, while the posterior approach is the most commonly used but spares the abductor muscles.7 Also patient position during surgery influences the success of the procedure, particularly in terms of acetabular cup orientation.8 However, the superiority of lateral or supine patient position is still debated. In daily clinical practice, this meta-analysis is useful for evaluating the pros and cons of each position (blood loss, operation time, limb length discrepancy and component placement) that must be evaluated when choosing a surgical approach. The aim of this systematic review and meta-analysis was to compare the supine versus lateral patient position in hip arthroplasty in terms of intraoperative and postoperative outcomes and component placement.
2. Materials and Methods
This study was carried out according with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. In this systematic review, we included studies that evaluated the role of patient surgical positioning on hip arthroplasty component placement and outcomes. We focused mainly on the patient’s decubitus for hip arthroplasty. Therefore, we included both studies that performed a similar approach in the two positions and studies that compared different hip approaches in the two positions.
2.1. Inclusion Criteria
The inclusion criteria were Cohort studies, Observational studies and Case Series (CS) in the English language, which compared the outliers of cup alignment for inclination and anteversion and intraoperative and postoperative clinical outcomes between supine and lateral position for patients who underwent THA. We excluded systematic reviews, nonhuman studies, studies in non-English language and studies that did not assess clinical or radiological comparison between the two patient positions.
2.2. Search Methods
The systematic literature research was performed by the use of Cochrane Central, PubMed–Medline, and Google Scholar, using the following search strings: “((arthroplasty, hip replacement[MeSH Terms]) AND (position, supine[MeSH Terms]) OR (supine[Title]))) AND (Hip[Title])” and “((arthroplasty, hip replacement[MeSH Terms]) AND (patient positioning[MeSH Terms])) AND (Hip[Title])”. The reference lists of the included studies were checked to achieve further eligible studies. After removing duplicates, two independent reviewers (G.P. and G.T.) checked the abstracts and subsequently read the full text of eligible articles in order to choose the included studies for this review and meta-analysis. Any divergence was discussed with the third review author (R.P.).
2.3. Data Collection, Analysis, and Outcomes
Two independent reviewers (G.P. and G.T.) performed the extraction of the following data: authors, year of publication, type of study, level of evidence (LOE), numbers of participants, with age, sex and body mass index (BMI) for both lateral and supine decubitus groups, diagnosis, procedure with kind of approach and follow-up. The component placement was assessed by cup inclination, cup anteversion and stem anteversion. Arthroplasty outcomes included blood loss, operation time, incision length, limb length discrepancy, hospital stay, Harris Hip Score (HHS) and Visual Analogue Scale (VAS).
2.4. Risk of Bias Assessment
Two reviewers (G.P. and G.T.) used the Methodological Index for Non-Randomized Studies (MINORS) score to evaluate the methodological quality of non-randomized studies. For comparative studies, as included in this review, it presets 12 items ranging from 0 to 2, for a total maximum of 24 points.
2.5. Statistical Analysis
A meta-analysis was assessed using the Review Manager (RevMan) software Version 5.4.1. The component placement was reported as odds ratio (OR) with 95% confidence intervals. For the calculation of the outliers of cup alignment, we considered the number of cups outside the target zone, which is represented by an inclination angle of 40◦ ± 10◦ and an anteversion angle of 20◦ ± 10◦. Hip arthroplasty outcomes, including both intraoperative and postoperative outcomes in lateral and supine position, were shown as mean difference (MD) with 95% confidence intervals. The heterogeneity was assessed by the I2 test. In cases of low heterogeneity (I2 < 55%), a fixed-effect model was used; whereas a random-effect model was performed for high heterogeneity. The statistical significance of the results was set at p < 0.05.
3. Results
3.1. Results of the Search
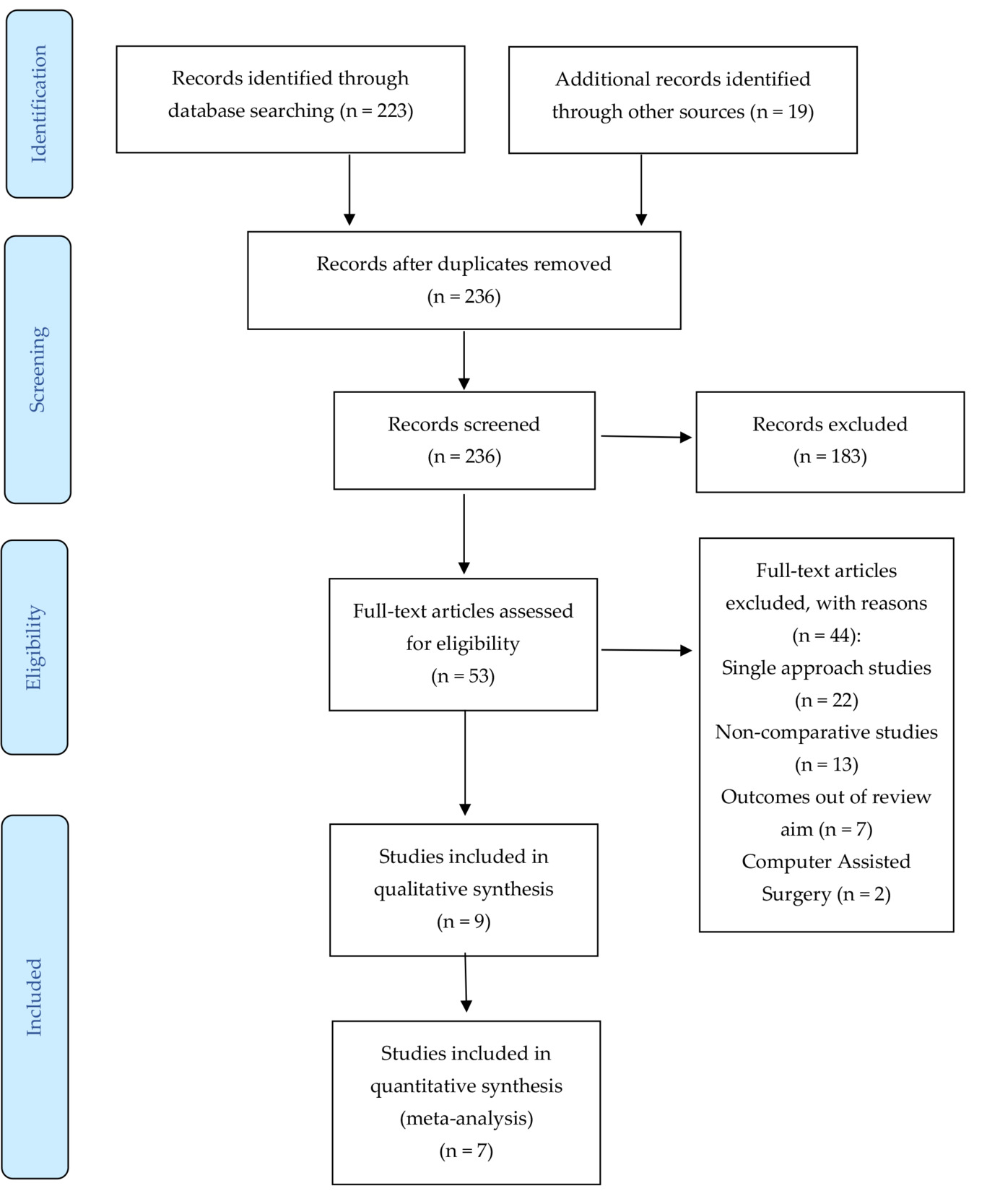
The literature search identified 242 articles. After the removal of duplicates, 236 studies were screened on title and abstract. Fifty-three articles were read in full text, and 44 of those were excluded for the following reasons: no positioning comparison, comparison of multiple approaches in a single positioning, navigated surgery, evaluation of out-of-focus outcomes. Thus, 9 articles were included in this review. Finally, 7 articles were included in the meta-analysis (Figure 1).
3.2. Included studies
The studies were one Randomized controlled study, 3 Retrospective Cohort Studies (RCS), one Retrospective Observational Study (ROS) and 4 retrospective Case Series. 4 studies focused more on component placement and outliers of cup alignment 8–11, while the other 4 studies evaluated mostly intraoperative and postoperative outcomes.12–15 The remaining study16 was not included in the meta-analysis due to the absence of the researched parameters.
3.3. Demographic Data
The overall number of participants was 662 in the lateral decubitus group and 509 in the supine decubitus group (Table 1). In 8 studies a Total Hip Arthroplasty (THA) was performed, while in one study13 the patients underwent hip Hemi-Arthroplasty (HA) due to femoral neck fracture (FNF), thus leading to the removal of this study from the meta-analysis. For the participants treated with THA the mean age ranged from 57.9 to 72.3 years. The gender distribution showed a prevalence of females, which ranged from 47.8% to 91.8% of the participants. BMI of the included patients ranged from 20.2 to 32.9. The approach used by the surgeon were: Direct Anterior Approach (DAA) in 4 studies, Direct Lateral Approach (DLA) in 3 studies, Posterior Approach (PA) in 3 studies, Anterolateral Lateral approach (ALL) in 3 studies, Anterolateral Supine approach (ALS) in 3 studies, Posterolateral approach (PL) in one study. The follow-up was reported in 5 studies and ranged from 3 to 35.4 month.
3.4. Clinical Outcome Data
For the component placement, cup inclination was assessed in 8 studies, cup anteversion was evaluated in 7 studies and stem anteversion was shown in 2 studies. Instead, regarding arthroplasty outcomes, HHS was evaluated in 3 studies, VAS was reported in 2 studies and Japanese Orthopedic Association (JOA) was shown in one study (Table 2).
3.5. Radiological Evaluation
In two studies9,10 radiography was not used to assess the intra-operative cup alignment. Instead, Grammatopoulos et al.17 produced an intraoperative anteroposterior (AP) pelvic radiograph both in lateral and supine position, after the introduction of the acetabular component. Finally, in the study by Takada et al.11 intraoperative radiographic cup inclination and anteversion were marked with a conventional manual goniometer. Moreover, Grammatopoulos et al.17 measured the inclination and anteversion of the acetabular component from the intra- and postoperative radiographs by a validated software. Kishimura et al.10 assessed post-operative up alignment and outliers using 3D-CT images. Takada et al.11 described the radiographic anteversion as the angle between the acetabular axis and the coronal plane, and the radiographic inclination as the angle between the longitudinal axis of the body and the acetabular axis projected on to the coronal plane. Finally, Innmann et al.9 performed 6-week postoperative radiographs and evaluated cup inclination as the angle between the transteardrop line and the line connecting the most superior and inferior aspect of the cup.
3.6. Methodological Evaluation
The (MINORS) score for the included studies ranged from 16 to 22, with a mean value of 19, showing a good methodological quality of non-randomized studies. More precisely, all the studies presented adequate aims, inclusion of patients, collection of data and endpoints. Moreover, all the articles analyzed adequate contemporary groups with baseline equivalence (Table 3).
3.7. Effect of Intervention
The meta-analysis was performed to evaluate intraoperative and postoperative outcomes and component placement between supine and lateral decubitus for hip arthroplasty.
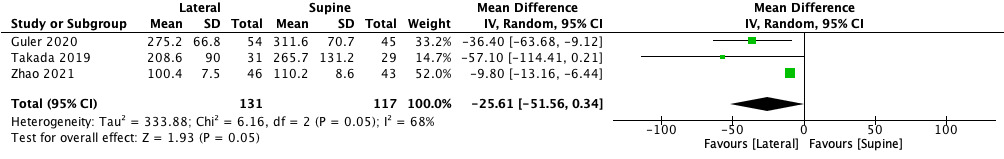
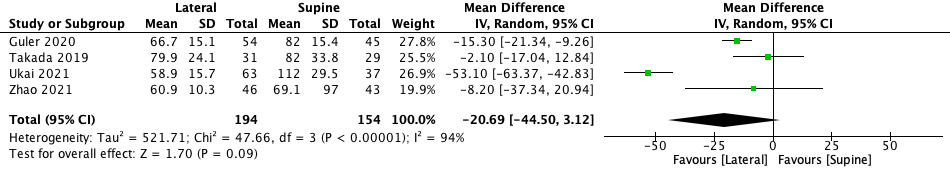
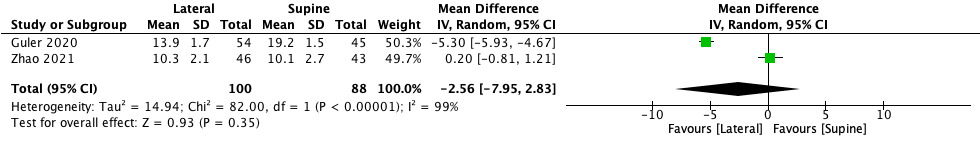
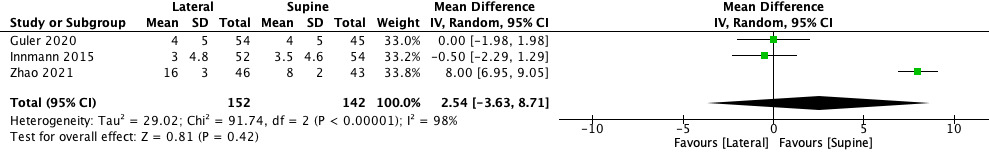
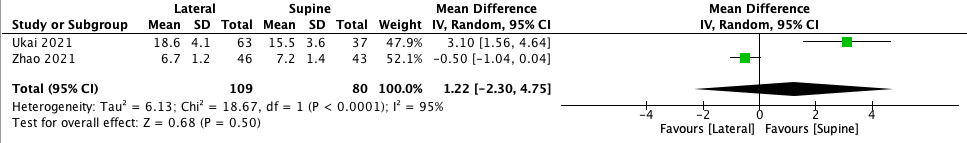
Blood loss resulted significantly lower in lateral position (MD −25.61, 95% CI −51.56 to −0.34, p = 0.05) (Figure 2). The operation time showed a shorter duration of surgery in favour of lateral decubitus (MD −20.69, 95% CI −44.50 to −3.12). However, the difference was not significant (p = 0.09) (Figure 3). The incision length was shorter in lateral position compared to supine position (MD −2.56, 95% CI −7.95 to −2.83), but there was no significant difference (p = 0.35) (Figure 4). Conversely, the limb length discrepancy was lower in supine decubitus (MD 2.54, 95% CI −3.63 to 8.71), without significant differences (p = 0.42) (Figure 5). Also the hospital stay was shorter in supine decubitus compared to lateral (MD 1.22, 95% CI −2.30 to 4.75), without significant differences (p = 0.50) (Figure 6).
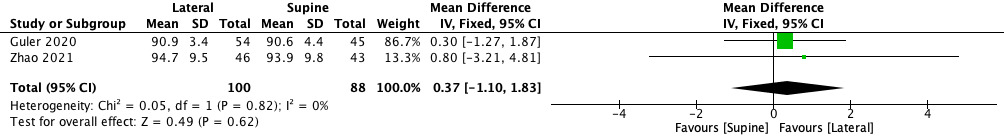
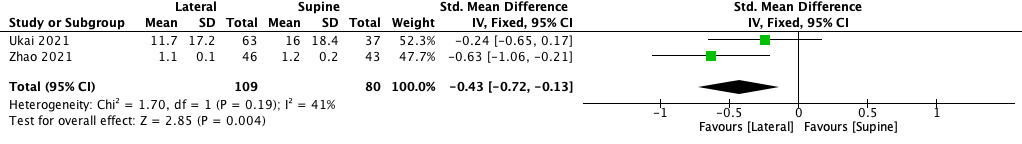
Regarding postoperative outcomes, HHS showed higher increase in lateral group (MD 0.37, 95% CI −1.10 to 1.83), therefore the improvement was not statistically significant (p = 0.62) (Figure 7). VAS showed a significant reduction of pain in lateral position (SMD -0.43, 95% CI −0.72 to -0.13, p = 0.004) (Figure 8).
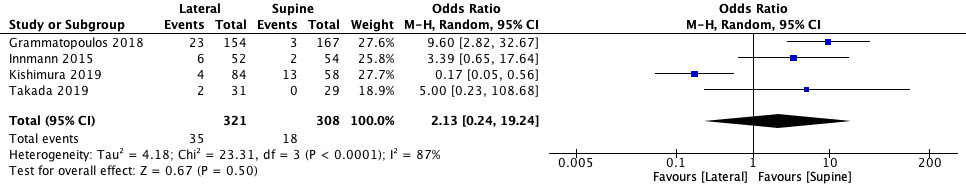
Regarding the component placement, the outliers for cup inclination were lower after arthroplasty in supine decubitus (OR 2.13, 95% CI 0.24 to 19.24), but there was no significant difference (p = 0.50) (Figure 9). Instead, the outliers for cup anteversion were significantly lower in supine position (OR 2.89, 95% CI 1.26 to 6.65, p = 0.01) (Figure 10).
4. Discussion
The aim of this study was to analyze the comparison between supine and lateral position for THA regarding intraoperative and postoperative outcomes and component placement. In line with current literature,18,19 blood loss resulted lower performing surgery in lateral position. Also, surgical time and the incision length were shorter in lateral decubitus, while limb length and hospital stay were lower in supine position, without a significant difference. Lateral position showed better results in terms of clinical outcomes, analyzing both Harris Hip Score and VAS scale, therefore the improvement in HHS was not statistically significant (p = 0.62). As regards complications, the number of intraoperative fractures and the rate of dislocations were lower performing lateral decubitus. In particular, Kamo et al.13 reported that supine position may lead to great trochanter fractures with a higher incidence compared to lateral decubitus, which rather causes periprosthetic fractures. Furthermore, we analyzed cup alignment, which is one of the main determinants of outcome in THA, with a recommended inclination angle of 40◦ ± 10◦ and an anteversion angle of 15◦ ± 10◦.20 Supine decubitus reported a lower number of outliers both in cup inclination and anteversion. In accordance with these results, Grammatopoulous et al.17 and Guler et al.12 deemed it easier to orient the pelvis anatomy with the patient in supine position, which permitted to achieve more accurate placement of the acetabular cup, also because of better pelvic stability. Even Takada et al.11 reported a higher accuracy in terms of radiographic inclination and a reduced risk of outliers (10° > aimed alignment) performing supine position in the anterior approach, without any significant difference in cup anteversion. On the contrary, Kishimura et al.10 experienced a higher rate of outliers of cup inclination using supine position, probably because of the use of a pelvic positioner during the surgery. Most of the studies reported no significant differences in femoral stem alignment comparing the two positions. Moreover, one of the benefits of the supine position is that allows the use of fluoroscopic image intensification that may help the correction and assessment component positioning during the surgery, leading to a more accurate alignment.21 Jil et al.16 indeed showed that fluoroscopy is more effective and accurate in supine position. Also, BMI plays an important role when choosing the patient’s position. Guler et al.12 found lower intraoperative outcomes using supine position compared to lateral decubitus in patients with body mass indices above 25 kg/m2. Zhao et al.15 also suggested treating obese patients in lateral decubitus, while supine position should be preferred in thin patients. Concerning the functional outcome, Wang et al.22 found an early functional recovery using the DAA approach instead of PL, while Ukai et al.14 reported better functional outcome, earlier use of cane and shorter hospital stays performing ALS approach over PL, although patients treated in ALS were more likely to experience weakness of the anterior hip muscles during the first 6 months after surgery. According to current evidence comparing outcomes of total hip arthroplasty performed with the patient in supine position versus in lateral position, we cannot make any firm conclusion on the superiority of either approach. Lateral decubitus showed better results in terms of intraoperative blood loss, surgical time, and incision length. Additionally, the use of this position also leads to better clinical outcomes and a lower risk of complications. However, supine position reported superior outcomes analyzing limb length, hospital stay, and number of outliers in terms of cup inclination and anteversion.
4.1. Limitations
The accuracy of the study may have been affected by the fact that some studies compared supine position versus lateral decubitus using the same surgical approach, while others included different approaches. Moreover, there were not enough studies to perform a subgroup analysis regarding only DLA, DAA or the comparison between ALL and ALS in order to achieve evidence. A limitation of the study was due to the presence of homogenous surgical indications in the studies. However, only one study in the meta-analysis included patients affected by FNF other than OA. Other confounding factors concerned the heterogeneity among the studies for the number of surgeons involved, the type of implants and fixation, which may alter the intraoperative outcomes, such as blood loss or operative time. Moreover, different anesthesia, pain relievers and rehabilitation may lead to bias in the postoperative outcome like VAS and HHS. Another limitation was represented by the absence of randomized controlled trials, due to the nature of the interventions. Therefore, apart from one randomized controlled study at level II of evidence, all the included studies were retrospective studies at III or IV LOE. Moreover, only 5 studies reported a follow-up, which was quite short, with a mean value of 14 months. Therefore, it was not possible to assess the long-term complications of the two different approaches, limiting the analysis only for intraoperative and perioperative complications.
5. Conclusion
This systematic review and meta-analysis showed no significant differences between the two groups for clinical outcomes, unless for blood loss and VAS, which presented statistical significance in favour of lateral decubitus (respectively p = 0.05 and p = 0.004). Regarding the number of outliers, the supine decubitus showed significant differences only for the cup anteversion (p = 0.01). However, more prospective studies with longer follow-up are needed to assess the superiority of supine or lateral patient position for THA. Moreover, studies should analyze both clinical and radiological parameters in order to lead to a complete evaluation of the correct decubitus position for each patient.
Author Contributions
Conceptualization, G.T. and R.P.; methodology, B.Z. and G.F.P.; software, E.A.; validation, B.Z.; formal analysis, G.T.; investigation, B.Z.; resources, G.F.P; data curation, G.T.; writing—original draft preparation, E.V.; writing—review and editing, G.F.P.; visualization, E.A.; supervision, B.Z. and V.D.; project administration, R.P.; funding acquisition, V.D. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding
This research received no external funding.