INTRODUCTION
Anterior Labroligamentous Periosteal Sleeve Avulsion (ALPSA) lesions can lead to chronic shoulder instability in active populations.1,2 The ALPSA lesion was first termed by Neviaser in 1993 as similar to a Bankart lesion except with an intact anterior scapular periosteum that causes the labrum to displace medially and inferiorly. These lesions can heal and ultimately cause recurrent shoulder instability due to a destabilization of the anterior inferior glenohumeral ligament.3 ALPSA lesions can occur in similar injury mechanisms to that of Bankart lesions,3 although ALPSA lesions may be more likely to occur as a result of repetitive dislocations rather than a single traumatic event.4–7 ALPSA lesions have repeatedly been identified as a risk factor for recurrent shoulder instability following arthroscopic Bankart repairs.1,2 Higher arthroscopic failure rates are also associated with ALPSA lesions compared to isolated Bankart lesions.4,7
To our knowledge, no systematic review has synthesized surgical outcomes or associated injuries following ALPSA lesion repairs. Therefore, the purpose of this review was to evaluate postoperative outcomes of ALPSA lesions, including recurrence rates, outcome scores, range-of-motion, return-to-activity, and surgical complications. These findings aim to provide a more comprehensive context for physicians and patients considering arthroscopic treatment for ALPSA lesions, as well as to highlight potential areas for future research.
METHODS
Literature and Database Search
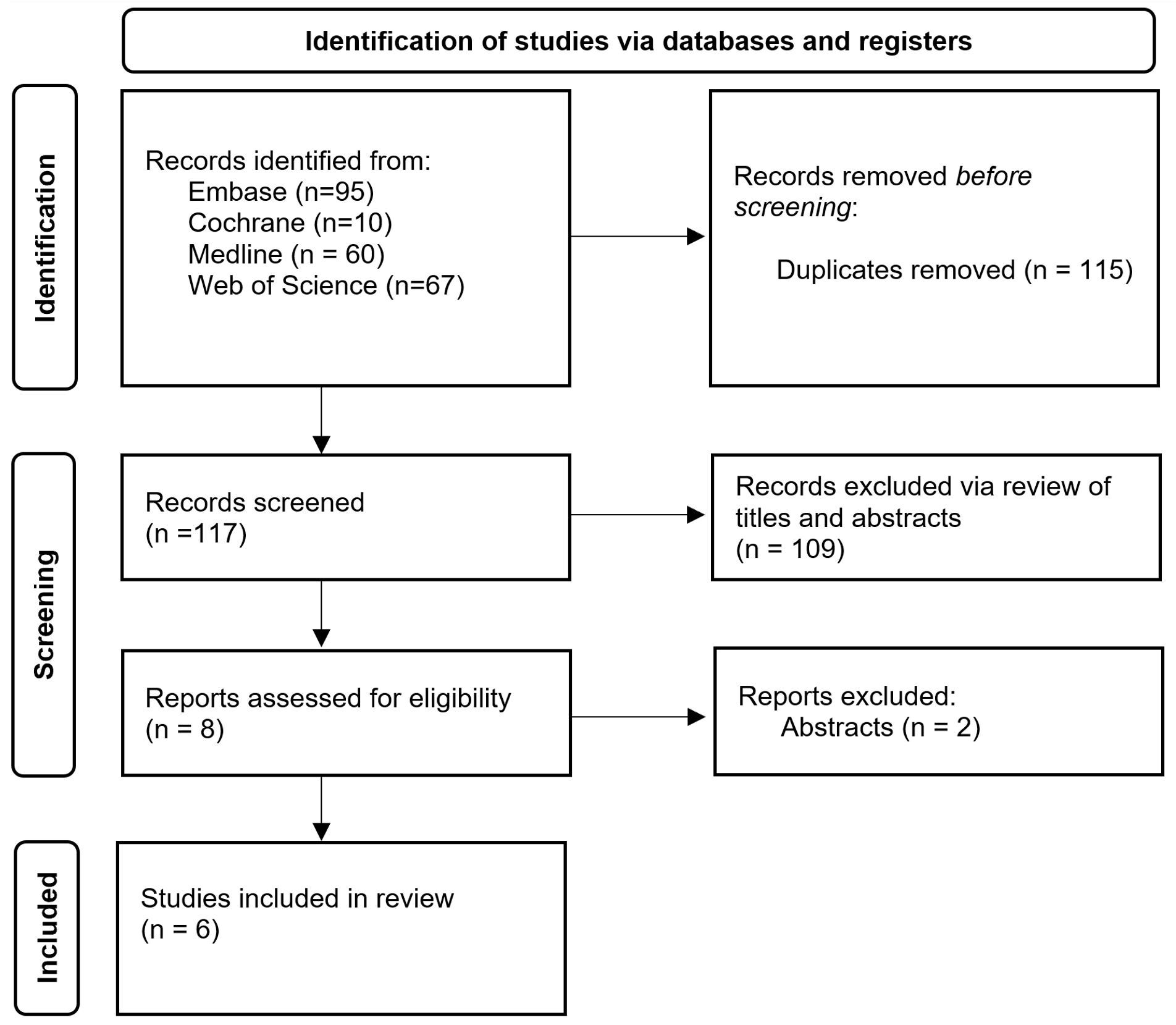
A systematic search of peer-reviewed, published literature was conducted in consultation with a research librarian in Medline (Ovid), Embase (Ovid), Cochrane, and Web of Science from the inception of the database to May 2022. The search was conducted with the keywords “ALPSA”, “anterior labrum periosteal sleeve avulsion”, “anterior labroligamentous periosteal sleeve avulsion”, and “anterior labral periosteal sleeve avulsion”. The full details of the search strategy and results for Medline, Embase, and Cochrane, and Web of Science can be seen in Appendices A-D, respectively. All references were imported into Endnote reference management software (Clarivate, https://endnote.com/) and duplicate references were removed, as shown in Figure 1. The remaining references were exported and uploaded to Rayyan (Rayyan, https://www.rayyan.ai/) for screening. The literature search and subsequent review was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) reporting standards.8
Eligibility Criteria and Study Selection
Two blind reviewers (CN, CR) initially screened title and abstracts of case reports, case series, cohort studies, and randomized controlled trials for inclusion. Included studies had to investigate management and outcomes of ALPSA lesions and be published in English. Studies were excluded if they did not directly investigate the management of ALPSA lesions. Non-human studies, non-English studies, reviews, technical notes, letters to the editor, and surgical technique papers were also excluded. Studies underwent a second full-text review based on the same criteria to exclude additional studies as needed. Any conflicts between reviewers were resolved through third-party consultations with a senior author (JS). Full details of the protocol for this systematic review were prospectively registered on PROSPERO and can be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022334855.
Methodological Quality Assessment / Risk of Bias
Methodological quality and risk of bias of included studies were assessed using the JBI protocol checklist for cohort studies, case series, and case reports, respectively.9 Each criterion consists of unique vetting questions that evaluate the validity of methods, appropriateness of analysis, and quality of presentation for their given study type. Two blind reviewers (CR, CN) reviewed each included study with any discrepancies discussed to reach a consensus. Any disputes were settled by a third reviewer (JS).
Data Extraction
For each included study, two authors (CR, CN) independently extracted data into a Google Sheets spreadsheet (Google LLC, Mountain View, California, United States). A second review of the extracted data was then performed by the opposite reviewer, with any discrepancies between reviewers being resolved through third-party consultation with a senior author (JS). Data for extraction from each study included study type, level of evidence, number of patients, sex distribution, mean age, surgical management, follow-up duration, surgical complications, associated injuries, and outcome parameters: recurrence rates, clinical outcome scores, and return to activity.
Statistical Analysis
Categorical variables were summated and presented as counts or proportions and continuous variables were computed for patient means. Outcomes of interest were tabulated to highlight the findings of individual studies. A meta-analysis was not performed.
RESULTS
Literature Search and Screening
The initial search yielded a total of 117 studies after duplicates were removed. After screening titles and abstracts for inclusion and exclusion criteria, 8 studies remained. 2 of the included studies were removed after full-text screening, leaving 6 included studies for data extraction. A flowchart in Figure 1 displays the results and reasoning of each screening step. All results were reported per the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) reporting standards.8
Methodological Assessment and Risk of Bias
Two blind reviewers (CR, CN) evaluated included studies for methodological quality and risk of bias according to the JBI Clinical Appraisal tools for cohort studies, case series, and case reports, respectively. Two cohort studies4,6 had a mean score of 10.5 out of 11. Three case series3,7,10 scored a mean of 9.3 out of 10 and one case report11 scored an 8 out of 8. All studies were deemed suitable for inclusion in this review.
Patient Demographics
The 6 included studies reported a total of 202 patients with sustained ALPSA lesions (Table 1). Of these patients, 117 were male, and 31 were female, with one study6 of 53 patients not reporting sex distribution of the ALPSA cohort. Patient ages ranged from 15 to 43 years. The mean patient age was 25.1 years, and one study3 reported an additional 23 patients listed ambiguously as less than 25 years.
Associated Injuries
There were 5 studies that reported associated injuries (all but Neviaser3). In these studies, there were a total of 192 reported associated injuries in 176 patients (Table 1) - a rate of 1.12 associated injuries per patient undergoing arthroscopic surgery to repair ALPSA lesions. Among the reported injuries, four injury types made up 94.27% (181/192) of all associated injuries. These included: Hill Sachs lesions (84, 43.75%), synovitis (35, 18.23%), SLAP tears (32,16.67%) and glenoid erosions or lesions (30, 15.63%). The remaining 6.25% of associated injuries included partial rotator cuff tears (3), full rotator cuff tears (4), loose bodies (4), osteoarthritis (3), and one count of a Bony Bankart lesion. Given that multiple associated injuries can exist per patient, and due to the studies being inexplicit in providing prevalence ratios for associated injuries, this study was not able to identify a definitive percentage of ALPSA patients presenting without any associated injury.
Management, Complications, and Recurrence
All 202 patients were treated operatively with an arthroscopic surgical technique (Table 1). No significant surgical complications were reported, with two studies3,11 specifying no complications were observed and the remaining 4 studies4,6,7,10 not commenting on complications. 26 patients (12.9%) experienced operative failure as indicated by the recurrence of shoulder dislocations. Patients were followed for a mean duration of 4.3 years with a range of 15 months to 13 years.
Outcome Scores, ROM, and Return to Activity
Four studies4,6,7,10 reported shoulder outcomes scores which can be seen in Table 1. Two studies4,10 of 90 patients had a mean American Shoulder and Elbow Surgeons Shoulder (ASES) score of 68.1 preoperatively and 89.89 postoperatively, while two additional studies6,7 of 79 patients reported a postoperative Rowe score of 85.5. Range-of-motion (ROM) data was available in 3 studies3,6,11 and outlined in Table 1. Neviaser3 found 26 of 26 patients to have a postoperative shoulder ROM identical to the contralateral shoulder, while Lee, Cho and Rhee6 measured a decrease in pre- versus postoperative external rotation. Only 1 study3 reported return-to-activity data and listed 26 of 26 patients had returned to their pre-injury activity level.
DISCUSSION
The goal of this systematic review was to outline associated injuries and postoperative outcomes of ALPSA lesion repairs. A primary outcome discussed in the studies was the recurrence rate of shoulder instability following operative repair. Our results found a 12.9% recurrence rate of shoulder instability among patients treated arthroscopically for ALPSA lesions. A recent meta-analysis found similar associations between ALPSA lesions and increased risk of recurrence. They reported that the presence of an ALPSA lesion was a significant risk factor for recurrent shoulder instability following arthroscopic Bankart repair.2 The recurrence rates after ALPSA repair in this study ranged from 3.8% to 32.0%, a comparable rate to that of Bankart repairs that ranged from 3.4% to 35% in a prior systematic review.1 However, two of the studies included in this review found higher rates of recurrence in ALPSA patient groups as compared to isolated Bankart groups.4,7 Despite these recurrence rates, physicians likely continue to perform arthroscopic ALPSA repairs due to the high frequency of preoperative dislocations in patients with ALPSA lesions, which was cited as over 12 dislocations per patient in one study.6 It should be noted however that the studies included in this review span nearly 30 years, during which time arthroscopic techniques have improved and different approaches to ALPSA repair have been developed.12,13 Ayoubi, Darwish, Saidy, Abdelnour, Maalouly, Aouad and El Rassi10 utilized a modified arthroscopic technique that elicited a recurrence rate of only 5% over 6 years of follow-up. It remains important for physicians to be aware of the recurrence risk when considering arthroscopic management of ALPSA lesions.
Aside from recurrence risks, ALPSA repairs still led to desirable functional outcomes, as evidenced by postoperative improvements in ASES and Rowe scores. ALPSA repair functional outcomes were found to occur with similar success to that of Bankart repairs with one study finding no significant difference in outcome scores between the two groups.4 Postoperative ROM differed amongst studies, with one study3 reporting full postoperative ROM and two studies6,11 citing limitations in shoulder abduction and external rotation. Varying surgical techniques may explain the discrepancy in ROM outcomes. Lee, Cho and Rhee6 suggested the postoperative loss of external rotation observed in their study may have been due to a tensioning effect of the repair on the capsule of the shoulder joint. Additionally, the effect of ALPSA repair on return-to-activity rates was not clear. Although one study3 reported a 100% RTS rate after ALPSA repairs, the body of literature regarding RTS rates after ALPSA repair was otherwise lacking. RTS rates, along with functional outcomes and recurrence risks, are all important aspects to consider before arthroscopic management and therefore more evidence of RTS rates would benefit decision making, especially for more active patients.
Our results additionally found that ALPSA lesions often occur with concomitant injuries, of which Hill Sachs lesions, synovitis, SLAP tears, and glenoid erosions or lesions were the most common. The development of concomitant injuries can likely be explained by the high number of preoperative dislocations experienced in patients with ALPSA lesions.6,14 Each subsequent dislocation increases stress on the shoulder joint space, which predisposes it to further injury. These findings may also be explained by the chronicity of ALPSA lesions. ALPSA lesions are more likely to develop in patients with recurrent dislocations than single primary dislocations.15 Therefore the associated injuries may predate the development of the ALPSA lesion. The presence of these associated injuries may contribute to negative outcomes and therefore identification of all co-pathologies is critical for effective treatment.16
The primary strength of this study is that it is the first systematic review to synthesize surgical outcomes of ALPSA lesions. This review spans 30 years’ worth of ALPSA research in over 200 patients. Our results serve to provide physicians with necessary information for arthroscopic management, decision making, and suggest key areas of further research needed, most notably return to activity outcomes. Additionally, recurrence rates serve as a key takeaway from this study due to the availability and homogenous reporting of such outcomes.
Our study is limited by the overall lack of literature surrounding ALPSA lesions, including only 6 studies that reported key patient outcomes and also met our inclusion criteria. Additionally, the broad time frame from which the studies were drawn makes our findings less generalizable to present-day outcomes which have likely improved in the past 30 years. Lastly, heterogeneous reporting of functional outcomes, with each study reporting a unique subset of outcome scores and ROM data, made true comparisons difficult and limited our ability to synthesize outcomes across all patients.
CONCLUSION
A systematic review of studies investigating ALPSA repairs found 6 studies of 202 patients from 1993 to May 2022. Arthroscopic ALPSA repair was found to produce satisfactory functional outcomes in patients. However, it is associated with a 12.9% risk of recurrent shoulder instability. Additionally, ALPSA lesions often occur with associated injuries - most commonly Hill Sachs lesions, synovitis, SLAP tears, and glenoid erosions or lesions. Further research is needed to evaluate the impact of APLSA lesions on RTS rates. Physicians should perform careful evaluation on patients with suspected ALPSA lesions to assess for the presence of co-pathologies. This can be an essential step in determining the appropriateness of arthroscopic repair for the treatment of ALPLSA lesions.
Author Contributions
CR: Design, Data Acquisition, Analysis, Interpretation, Drafting, Final Approval
JS: Conception, Design, Analysis, Interpretation, Drafting, Final Approval
MJ: Conception, Design, Drafting, Final Approval
CN: Design, Data Acquisition, Analysis, Interpretation, Drafting, Final Approval
JC: Design, Data Acquisition, Final Approval
AV: Conception, Design, Interpretation, Drafting, Final Approval
Disclosures
The authors have not received any grant support or research funding for this study and have no proprietary interests in the materials described in this article.
Further Information
No external funding was received for this study.