Introduction
Primary total knee arthroplasty (TKA) is an effective treatment which is increasing in use for both elderly and younger patients. Coupled with the overall increasing life span of the general population, the rate of revision TKA is also projected to increase significantly over the coming decades.1 Analysis of the national joint registry of England and Wales has predicted an increase in primary TKA of 117% and an increase in revision TKA of 332% by 2030.2 This is based on the volume of procedures from the time period of 2008-2012, and data from the office of national statistics allowing a projection of population to the year 2030.3
Indications for revision TKA
The British Orthopaedic Association (BOA) has recently released guidance on investigation of problematic TKAs, with surgically correctable causes summarized by the acronym “SPECIFIC”4:
-
Stiffness and Soft tissue problems (wound breakdown, synovitis, impingement, haemarthrosis)
-
Patellar / component malposition / component malrotation
-
Extensor mechanism dysfunction
-
Component loosening
-
Infection
-
Fracture
-
Instability
-
Component wear / breakage
These indications are recorded in the National Joint Registry of England and Wales (NJR).5 The reasons for failure of primary TKAs have been analysed using data from national registries. The National Joint Registry of England and Wales (NJR) shows 35% of revisions are for aseptic loosening, 23% for infection, 14% for instability and 20% for wear. This is comparable to other large joint registry findings from Australia and Sweden.6 Registry data from the USA lists infection as the most common reason for revision (20.4% of 337597 patients), closely followed by aseptic loosening 20.3%, with instability as 7.5% and wear as 2.6%.7 Polyethylene wear leading to aseptic loosening has historically been the most common overall reason for revision, in up to 44% of cases, and commonly occurring as a late (> 2 years) complication.8 Advances in polyethylene production, including highly crosslinked polyethylene and improved packaging to reduce oxidisation, have lead to significantly increased resistance to wear.9 The rising use of unicompartmental knee arthroplasty has also contributed to rising rates of revision TKA, as they can have up to 4 times the revision rate of an unconstrained TKA. Factors such as component malpositioning, postoperative limb malalignment and surgeon volume are thought to contribute to this.10
Bone loss in TKA
Bone loss presents a challenge in revision TKA so an understanding of the aetiology and principles behind this is essential for the surgeon undertaking revision. The main mechanisms are as follows:
Stress Shielding
Stress shielding refers to the reduction in loading on a region of bone due to an adjacent implant. As a consequence of this reduced loading, bone is lost and there is a decrease in the bone density in this ‘shielded’ region next to the implant. This process of the bone remodelling according to the mechanical load placed upon it, is in keeping with Wolff’s law and Frost’s mechanostat hypothesis.11 In relation to the TKA, the bone directly beneath the tibial or femoral prosthesis can become osteopenic as a result of the implant directing the load through the implant into the diaphysis of the bone, leading to epiphyseal and metaphyseal bone loss.12 Biomechanical studies using finite element analysis (FEA) have shown that implant material properties play a significant role in stress shielding. Stiffer implants, such as those with cobalt chrome tibial baseplates, have been shown to have a higher degree of stress shielding than all polyethylene tibial baseplates which are made of a more elastic material.13 Stemmed prostheses further suffer from stress shielding, as while they improve implant stability in the form of resistance to shear forces and tibial lift off, this comes at a cost of stress shielding from the stem with associated osteopenia, leading to risk of implant displacement and periprosthetic fracture.14
Aseptic loosening, wear and osteolysis
Mechanical loosening (aseptic loosening) is the leading cause for knee revision in the United Kingdom. There are many mechanisms which contribute to this: high loading of the bearing surfaces, exacerbated by component malalignment, prosthesis instability and patellofemoral maltracking.15 This leads to the production of particulate wear, which in turn activates macrophages expressing inflammatory mediators (chemokines, cytokines, reactive oxygen and nitrogen species, prostaglandins). This in turn leads to an increase in the number of activated osteoclasts at the bone – implant interface and subsequent bone resorption.16
Simultaneously, inflammatory signals direct the growth of a pseudo-synovial tissue and granulomatous tissues, which secrete large amounts of fluid into the joint space. This can lead to increased hydrodynamic pressure within the joint cavity. This can cause direct damage to the spongy peri-implant bone surface inducing osteocyte death and debonding of the implant or cement interface.17
Historically wear was the leading cause for TKA revision,18 however this is no longer the case as there have been significant advances in every aspect of both polyethylene and metal components of the TKA. There are fewer problems with excessive loading due to component mal-positioning as the understanding of knee biomechanics has lead to significant improvements in operative technique, with mechanical, kinematic and anatomical alignment methods.19 Furthermore there have been improvements in locking mechanisms of tibial inserts and reduction of backside wear.20 The polyethylene manufacturing process has improved, with the development of newer highly cross-linked PEs (HXLPEs) and the introduction of additives, such as vitamin E.21 Metalosis of either the femoral component or tibial tray generates a similar debris and inflammatory response and if present acts in combination with polyethylene debris to contribute to wear induced osteolysis.22 Failure of the TKA can often be multifactorial, with wear and loosening co-existing, therefor detailed intraoperative implant scrutiny must be made to ensure the most appropriate operation or revision strategy is used.23 Isolated tibial insert exchange has been shown to be reliable when used for insert wear alone.23
Infection
The development of prosthetic joint infection (PJI) and its subsequent treatment with options such as debridement and revision surgery can lead to significant bone loss.
During active infection, bone loss ensues as a result of direct toxin related damage from the infectious organisms, with subsequent host inflammatory and immune complex responses. In cell culture models of osteomyelitis, the site of infection by Staphylococcus aureus was observed to have high numbers of both macrophages and osteoclasts. Infectious bacteria produce a wide variety of enzymes and toxins resulting in enzymatic degradation, activation of fibrinolytic activity, vascular damage and subsequent bone necrosis. The immune response leads to release of antibodies and cytokines, which in turn activate osteoclasts and result in bone resorption.24 However this was a cell culture based study, in animal this may not happen otherwise we would not have sequestra – they would all have been resorbed. Wang et al have shown that some products from staph inhibited osteoclasts.25
At operation, a thorough and systematic debridement of infected and non-viable tissue is required to maximise the chance of success. At this time, the implant may be loose and easily removed, however in infected cases26 the remaining cement mantle must be removed, which can result in significant bone loss.27 Uncemented implants which have not become loose can also be extremely difficult to remove without inducing bone loss.28
There are separate challenges arising with regard to the cement spacer in a 2 stage procedure. The purpose of the spacer is to deliver a high concentration of antibiotic locally, and to try and preserve joint space and tissue tension.29 Complications of the spacer can include quadriceps scarring, arthrofibrosis, bone loss and spacer dislocation.30 The bone loss is due to invagination of the spacer into the soft remaining bone (often due to undersizing of the spacer) and erosion at the bone – spacer interface due to shear movements. Bone is also lost, as a result of disuse osteopenia as often these patients will be non-weight bearing on the affected limb. Finally, bone can be lost due to the immune response to wear particulates.31 Some of these issues have been improved with articulating spacers, which allow partial weight bearing, a degree of flexion in the joint and more appropriate moulds to prevent under sizing related bone loss.30 Complications due to spacer subluxation and dislocation has been reported to occur in up to 12% of cases, leading to fracture and in some cases dislocation of the knee.32 Lau et al investigated the effects of spacer subluxation and dislocation in revision TKA. They reported that increased tibial and femoral bone loss can occur with spacer displacement, as well as higher rates of re-infection and a need for a higher level of constraint of the definitive implant at the second stage of revision.33
A novel method for avoiding these issues is the use of custom made articulating spacer (CUMARS). This technique was initially used in 2 stage revision hip arthroplasty and describes loosely cementing definitive implants, the cement is used in the doughy stage to conform to macroscopic architecture of the bone, rather than microscopic interlock with cancellous bone.34 The authors described eradications of infection in 84.2% of cases which was comparable to both 2 stage and singe stage revisions in a systematic review.35 Proposed advantages are improved function, retained soft tissue tension and improved patient tolerance in the period between staged revisions. 44.7% of patients in their series indefinitely postponed the 2nd stage of revision due to good function.34 Matar et al report 22% of patients planned for 2 stage revision indefinitely postponing the 2nd stage due to success of the CUMARS.36 Marson et al investigated this technique for TKA and found it effective in allowing full weight bearing and maintaining knee flexion, they had no-reinfections. They comment in some more frail patients with lower demand it can be a definitive treatment, however second stage of revision can subsequently be performed if necessary.37
At the second stage revision procedure there can be some bone loss when removing a spacer if interdigitation with bone has taken place and as a further targeted debridement/resection is undertaken as the tibia and femur are prepared to accept their definitive implants.
Classification of bone loss in TKA
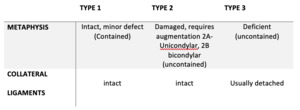
After establishing the reason for failure, a further critical step in pre-operative planning is assessment of bone stock and bone loss. This can initially be done on pre-operative radiographs, however final intra-operative assessment may reveal more substantial loss.28 Engh et al described the Anderson Orthopaedic Research Institute (AORI) classification which has now become the most broadly adopted classification system globally. This defines the bone loss as tibia (T) or femur (F) independently, and the severity is graded 1 to 3. 1 is a minor defect at the level of the bone-implant surface, with no significant defect extending into the metaphysis, implant stability is not compromised. Type 2 has metaphyseal damage which required adjunct for stability, this can be further split into 2A – when one femoral condyle or one side of the tibial plateau is affected, or type 2B – both condyles or both sides of the plateau.38 Type 3 is deficient metaphysis, with major loss of plateau or condyle, often with ligamentous detachment39 (figure 1) (table 1). The term contained describes a central bone loss with intact peripheral cortical rim surrounding it, uncontained describes a defect in the cortical rim.40
Morgan-Jones et al have described the zonal classification of fixation in revision TKA. They describe within the knee, 3 anatomical zones in which fixation can be achieved. Zone 1 is the epiphysis, zone 2 the metaphysis and zone 3 the metaphysis.41 The classification provides a system for pre-operative planning and advises that stable fixation is required in at least 2 of the 3 zones (figure 2). The surgeon can use this working methodology to select the most appropriate adjunct and or implant for managing bone loss in each case.
Strategies for management of bone loss
Various methodologies for the management of bone loss in revision TKA have been proposed: cement, bone graft, modular metal augments such as wedges, metaphyseal fit implants (cones and sleeves) and endoprostheses.
Cement
Cement is readily available, inexpensive and highly conformable to the size and shape of a defect, with the added ability to deliver local antibiotics. It does however have the risk of causing thermal necrosis to the surrounding bone, which may lead to osteonecrosis and implant instability. There are further risks of stress shielding to surrounding bone due to poor load transfer, limiting its long-term suitability. It can be used for treating defects <5mm42; in a series of 59 knees followed up for mean 7.1 years, only 1 patient required revision, however 43 cases showed some non-progressive radiolucency.43
Cement can be augmented with screw fixation and used for AORI type 1 and 2(small and uncontained) defects. This technique has been shown to have excellent results at 13 years with no failures (screw and cement). It is not recommended for defects >10mm or patients with poor quality bone.44
Bone grafting
Bone graft can be autograft or allograft. Autograft is often harvested from distal femur, iliac crest or contralateral tibia, and has the gold standard properties of osteogenicity, osteoinductivity and osteoconductivity,.45 There is potential donor site morbidity which can include wound issues, blood loss, chronic pain and infection.46 The alternative option is allograft, however this exchanges donor site morbidity for different risks including reduced strength due to the gamma radiation sterilisation process, immune rejection, delayed union and disease transmission.47 Bone grafting is generally not suitable for revisions for infection.
Impaction bone grafting can use either type of graft, used with or without a mesh adjunct for containment. The bone is morselized and added to deficient area to build up bone stock. The process is time consuming and technically challenging, it involves meticulous preparation of the bone graft and host.48 Due to this and because the biological response of condensed bone is variable,49 impaction grafting remains a controversial treatment method, with great variability in operative technique and style of revision knee implant used. The numerous techniques suggest an ideal solution has not yet been reached. Whiteside reported excellent results of 105 patients who underwent this technique in conjunction with a long uncemented stem, showing only 1 case of aseptic tibial loosening with follow up between 5-10 years.50 Diaphyseal engaging stems have been shown to decrease proximal graft loading by up to 38%,51 with some authors proposing a shorter stemmed implant engaging with the graft is superior.52
Bulk structural allograft is an alternative technique used to address larger and uncontained defects. It is frequently performed with femoral head allograft meticulously trimmed of fibrous tissue and cortical bone, then treated with pulse lavage to remove marrow. The receiving bone is prepared with an acetabular reamer, and the allograft fixed in place with cancellous screws.53 Risks of this technique are non-union of the graft and collapse due to resorption with subsequent implant displacement. This technique has been shown to have variable survivorship rates from ~70% at 1 year in a series of 2654 and ~70%55 at 10 years in a series of 50 when re-operation for any reason is used as an end point. Histological analysis has been performed during re-revision surgery and from cadaveric retrieval, demonstrating whilst allograft may have not resorbed, there was no evidence of revascularisation or of incorporation into the host bone.56
Metal Augments
Both femoral and tibial components can have metal augments attached to their under surface and are available in the form of blocks and wedges, symmetric or asymmetric.57 They can be attached using cement or screws, allowing up to 20 mm of segmental bone loss to be replaced and offer immediate support with satisfactory transfer of load.58 Augments are readily available, quick to assemble, and their modularity allows for correction of alignment in coronal plane and re-establishment of the anatomical joint line.59 Some additional resection of otherwise normal residual bone stock may be needed to facilitate their placement, and there is a potential risk from corrosion and wear debris resulting from fretting between the implant and the augment. Stress shielding of metaphyseal bone remains a concern.60 Blocks have been seen to perform better than wedges in biomechanical studies; Wedges demonstrate increased shear forces leading to loosening, whereas blocks subject the underlying surface to compression forces.61 Hamai et al reported good mid-term results using blocks with an 8% failure rate in their series of 26 patients with a mean follow-up of 6 years.62 Hockmen et al found in 48% of cases additional bone grafting was needed to address the bone loss comprehensively.58 The overall literature lacks long term and large scale studies on this area of revision total knee arthroplasty.
Megaprostheses
A megaprosthesis , or endoprosthesis, is used when the bone loss is not reconstructable, and the aim is joint salvage allowing the entire proximal tibia or distal femur to be replaced. The main advantage is preservation of joint and limb to allow ambulation. Limitations of these implants are high soft tissue failure rate, infection, poor function, implant and periprosthetic fracture.63 Their initial use was post en-bloc tumour resection, with favourable outcomes shown in terms of return to ambulation.64 There has been increasing interest in their use for highly comminuted intra-articular fractures of the distal femur and proximal tibia, where reconstruction may not be the most appropriate treatment option, and now in as a salvage procedure for revision knee replacement. Periprosthetic and inter-prosthetic fracture rates are increasing65 and whilst internal fixation with a locking plate or intramedullary nail are often the preferred initial treatments, poor bone stock can ultimately lead to failure.66 In these instances, distal femur replacement and proximal tibia replacement remain effective salvage procedures in, as they have been shown to have equivolent results to open reduction and internal fixation.67 }
The literature for endoprosthetic use in revision TKA is however limited. Survivorship rates in a series of 56 have been reported as 75% at 5 years and 56% at 10 years for the cemented stems .68 In comparison in a series of 50 uncemented stems, 94% survivorship at 5 years has been reported, with no 10 year data available.68
Concerningly, studies in the literature report significantly increased infection rates for megaprostheses used for oncological surgeries (29.5%), however the infection rates when used for revision knee surgery have been shown to be substantially lower (9.1%).69 Megaprostheses can be seen as a “last resort” treatment option to avoid amputation of the limb.70
Metaphyseal fit implants
The variable results of the aforementioned techniques has lead to the advent of metaphyseal fit sleeves and cones. As the name suggests both techniques act to transfer load to surrounding metaphyseal bone in the hope of gaining more stable fixation and reducing stress shielding.71
Cones are made of either tantalum or titanium, they are ultraporous, meaning they have interconnected pores of size 500 to 600 nanometres leading to 60% to 65% overall porosity depending on the individual implant72 (figure 3). They promote osseointegration, allowing the cone to be implanted with an uncemented technique to address cortical rim bone loss. The material of the cone has a Young’s modulus of elasticity closer to that of cancellous bone than solid metal, which facilitates load transfer to the remaining metaphyseal bone avoiding stress shielding. In simple terms it can be thought of as a metaphyseally anchored, metallic bone graft.73 Any remaining space between the cone and host cortical rim can be filled with bone graft or substitute.74 The definitive revision TKA is then placed within the cone with a stemmed prosthesis.75 There is no clear benefit to a cemented or uncemented stem, however using an uncemented stem can be technically challenging as offset couplers cannot be used due to the cone which may lead to malalignment of the component.76 Due to the highly osseointegrative properties of the cone, a limitation of the cone is bone loss during any subsequent removal for situations such as infection.77 A long-term follow-up (minimum 10 years) has shown 75% survivorship of 32 cones, with failure defined as revision for any reason. Reasons for failure were aseptic loosening (15.6%), infection 9.4%.73
The alternative metaphyseal fitting implant is the porous coated sleeve (figure 4). Metaphyseal sleeves are stepped and coated with titanium beads allowing for bone ingrowth. The sleeve is then combined with a Morse taper junction to either the femoral or tibial component. Surgical technique involves reaming the host bone to accept compaction broaches which are sequentially increased in size until rotational and axial stability are achieved during on table testing.78 The sleeves can be used with or without an intramedullary stem, which in itself can be cemented or press-fit.79 Advantages of this technique are rotational stability due to the stepped design, highly osseointegrative coating and immediate loading of metaphyseal bone to prevent stress shielding. Limitations are once again difficulty in removal and risk of intra-operative fracture during broaching.80 Bloch et al reported favourable results using this technique with 97.8% survival at 10 years of 73 implants. They report 5 failures (defined as re-revision for any reason), 4 for infection and 1 for instability.81
Conclusion
This article discusses the 3 main mechanisms for bone loss during revision TKA: stress shielding, aseptic loosening and infection. The Anderson Orthopaedic Research Institute (AORI) classification and zonal classification systems have been described and the current main methodologies for addressing the bone defects in each group have been discussed. Knowledge of these principles and techniques will benefit surgeons in their understanding of the options available to them, maximising their ability to give the patient a high performing revision TKA.
Conflicts of Interest
There are no conflicts of interest from any author to report
Sources of funding
There are no sources of funding from any author to report.