Introduction
Anterior cervical discectomy and fusion (ACDF) is the most commonly performed surgical intervention for the degenerated cervical spine. Clinical and radiological outcomes are favourable and Serious Adverse Events related to the procedure and used stabilisation devices are rare.1–7 Goals of ACDF include thorough decompression of the neural elements and obtaining solid arthrodesis. Although ACDF generally has a low complication rate, pseudarthrosis remains a common complication and may lead to revision surgery.8–10 As the use of autograft alone produces a variety of complications (i.e., graft settling, graft compression fractures, graft dislocations, pseudarthrotic segmental healing, and kyphotic segmental deformations) anterior plate fixation was introduced to augment interbody stabilisation in an effort to provide immediate short-term stability and avoid the necessity for external immobilisation, and potentially decrease pseudarthrosis rates.2,8 For the first generation of plates, with screws not firmly attached to the plate, implant-related complication rates were as high as 22–44 %.11 The next generation of plates introduced enabled successful angle stable fixation of the screws, allowing the screws to be firmly attached to the plate. However, further studies revealed an unfortunate tendency to detach themselves from the bone.12 The next progress in technological development of cervical spine plate designs is the dynamisation of such implants.13,14 This design allows screws to glide toward each other in the postoperative process of graft settling.15 Moreover, the design of the screws prevents loosening.16 These plates are commonly known as dynamic plates. A systematic review of five studies found a similar clinical outcome in ACDF for one-level fusion patients with dynamic and rigid plates, although the hardware failure rate was higher in ACDF with rigid plates.17
The local institutional ethics committee gave consent to this follow-up study under registration number 2019-14534-MPG § 23b and approved conformity of the study to the Helsinki Declaration and to local legislation. The study is registered under ClinicalTrials.gov ID: NCT04489394 .
We intended to assess minimum one-year clinical and radiological follow-up results of a third-generation anterior fixation device in our institution.
Materials and Methods
Surgical procedure
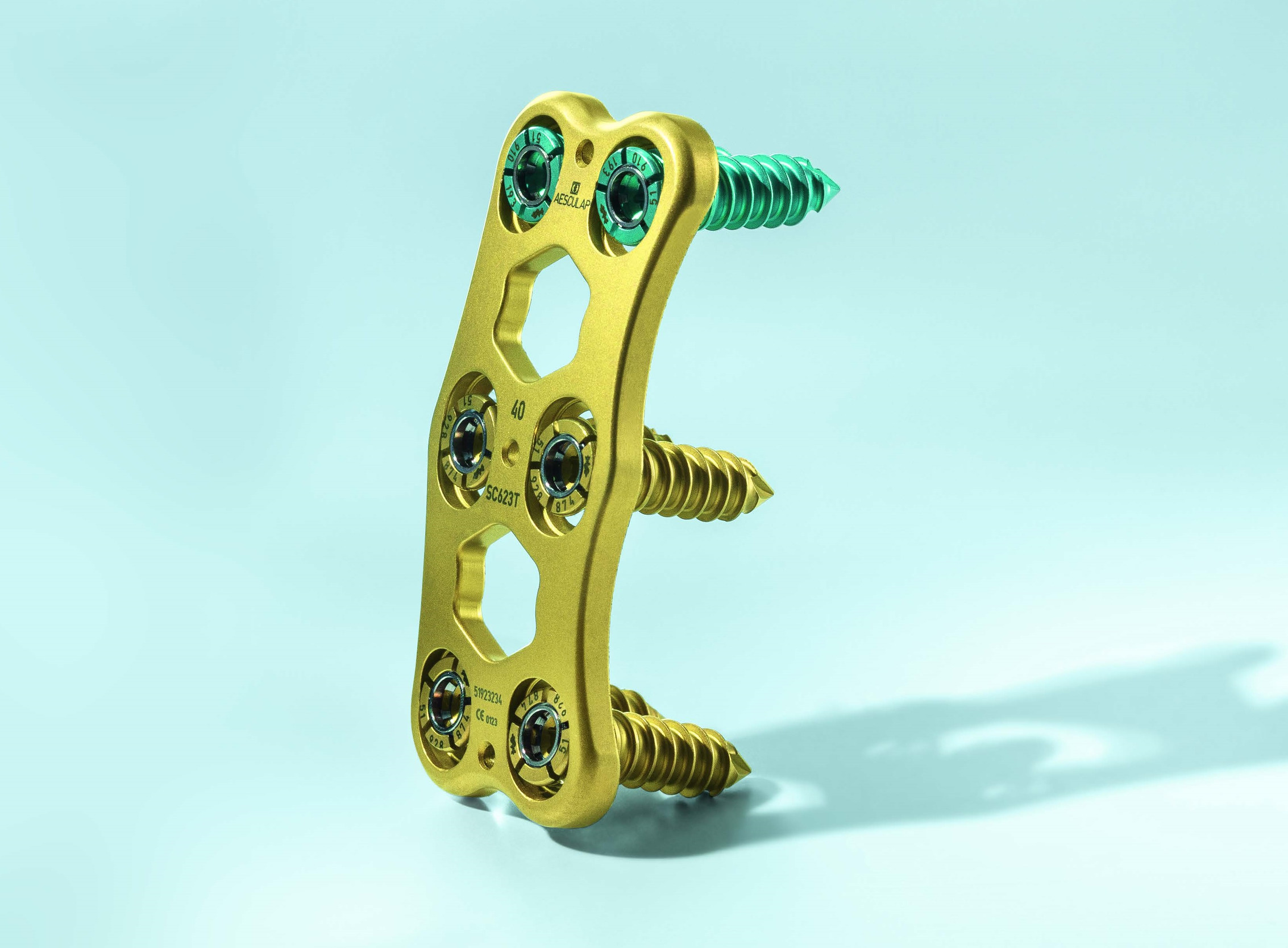
ACDF was performed in supine position by a transverse skin incision from the right side after introduction of general inhalation anaesthesia. All operations were performed by experienced spine surgeons (BB, GR, DB, FK).The surgical approach followed the classical Smith-Robinson-procedure.18,19 In all cases, a radical microsurgical discectomy was performed, including resection of potential posterior osteophytes, extraction of any disc extrusion as well as a thorough preparation of the end plates including a complete discectomy using various rongeurs, box and bone curettes, and decompression of the nerve structures. The posterior longitudinal ligament was opened transversely to expose and clearly visualise the dura. Interbody fusion was performed with a PEEK cage, uncoated (Fidji® PEEK Cervical Cage, Zimmer Spine, Bordeaux, France) or titanium-coated (Cespace® XP, BBraun Aesculap, Tuttlingen, Germany). Cage height was generally oriented to the height of the adjacent segments and the sagittal profile. After the cage was implanted, an anterior plate fixation with a dynamic cervical plate was added (Quintex®, BBraun Aesculap, Tuttlingen, Germany, see Figure 1). The correct position was checked by anteroposterior and lateral views of plain radiography before wound closure. After the surgery, patients were mobilised immediately and followed-up clinically and radiologically at least until one year after surgery. After that they usually come back if they experience any Adverse Events.
Clinical and radiological examinations
Inclusion and exclusion criteria were applied to all patients who received a Quintex cervical plate. Follow-up examinations were performed on an outpatient basis in our department. If a physical examination in the hospital was not possible and inclusion criteria were met, patient reported outcome measure (PROM) questionnaires were sent out by mail, including a consent form to be signed.
Functionality was assessed with help of the validated German Neck Disability Index forms (NDI). This assesses neck-specific function with a point value (0-50 points), or a percentage (0%–100%; where 0, or 0% denotes optimal function).20,21
The categories were defined according to the Physiopedia categories for the NDI, (0-4 points (0-8%) no disability, 5-14 points (10 – 28%) mild disability, 15-24 points (30-48%, moderate disability, 25-34 points (50-64%) severe disability, 35-50 points (70-100%) complete disability.22
As cervical spine procedures carry a non-negligible risk of swallowing irregularities, a separate dysphagia index, the Bazaz score, was added to the questionnaires.23,24 Additionally, residual neurological deficits and how the situation compares to the preoperative state were assessed.
Further, patients were asked if they would do the surgery again.
Adverse Events and serious adverse events were collected from the patient files. The patients were then asked if they experienced any medical events. They were encouraged to report the full picture, related or not related to the index surgery.
Radiological analysis involves preoperative, postoperative and follow-up standard anterior-posterior and medial-lateral X-rays. Flexion and extension X-rays were not done, as they are not part of the radiological standards in the hospital. The results were either collected at one-year follow-up, or at the invited follow-up for this study, in cases where the regular one-year follow-up visit with X-ray exam was missing. Computer tomography and magnetic resonance imaging MRI were not regularly done. The analysis includes a qualitative check of bone quality regarding density and sclerotic findings, evaluation of fusion criteria as visibility of anterior and posterior bone bridges or densities between adjacent vertebral bodies, and presence or absence of scleroses or radiolucent lines along the screws’ implant-bone interface. Further, an evaluation was performed of the intraosseous anchoring of the plate screw construct as well as for signs of loosening. Measurements were done on digital X-rays.
Statistical analysis
All values were expressed as mean with standard deviation. The statistical evaluation was performed using SAS Software version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical analysis of age, gender and further baseline characteristics and outcomes was performed with Student’s t-test.
Results
After checking the inclusion and exclusion criteria in 180 patients who underwent ACDF surgery with the dynamic anterior plate Quintex between 2014 and 2019 at our hospital, 62 patients fulfilled the inclusion criteria at first sight, and were contacted. Two patients refused to participate in the study due to lack of interest. The remaining 60 subjects agreed to cooperate in assessing the mid-term results of their anterior fusion surgery. Twenty-six patients came for a physical examination to the hospital, and 34 filled out the PROM questionnaires and sent them back to the hospital together with a written and signed Informed Consent. Demographic data was then extracted from the patient file for the 60 cooperating patients.
Thirty-three men (55%) and 27 women (45%) participated in the study. The average age was 58.8 years at surgery (26-77, STD 10.4). The average BMI was 28.1 (18.9-37.9, STD 5.0). Forty patients never smoked (66.7%), four did but then quit (6.7%) and 16 were currently smokers (26.7%). Major reasons for needing cervical surgery were spinal stenosis in 54 cases, and 18 cases of manifest degenerative disc disease defined as “cervical pain of discogenic origin with historically and radiologically confirmed disc degeneration”. Further, indications mentioned less frequently were a failed previous fusion (3 cases, 5.0%) and (one case each, 1.7%) spondylolisthesis, trauma (fracture or dislocation), deformity (e.g. scoliosis, kyphosis and/or lordosis), pseudarthrosis as a result of a failed spinal surgery, symptomatic cervical spondylosis, instability after surgery due to one of the previous indications, a block vertebra formation, a pre-operation of cervical segment C5/C6, and a ventral fusion of the cervical segment C4/C5 and concomitant bleeding and haematoma.
The patients came with various risk factors that were documented in detail (Table 1). Only six patients had no documented risks at all, the others up to six risk factors, 2.13 risk factors per patient on average. The most common concomitant diseases mentioned are cardiovascular 37 times (29%), other orthopaedic issues (17, 13%), thyroid problems, mostly hypothyroidism (14, 11%), metabolic diseases (12, 9%), neurologic issues (8, 6%) pulmonary problems (8, 6%), diabetes (7, 5%), and abdominal (5, 4%). Other risk factors (21, 16%) were allergy (3), cancer (3), vascular (3), dermatologic (2), infectious disease (2), obesity (2), nephrologic (2), gastroenterological (1), nose surgery (1), ophthalmological (1), pain (1).
The total of segments treated in the 60 patients was 167, this corresponds to 2.8 levels treated per patient on average (one level:4 (7%), two-level: 17 (28%), three-level: 28 (47%), four-level: 10 (17%), and only one five-level case, (2%).
The most frequently treated segments were C5/C6 with 57 (34.1%), C4/C5: 46 (27.5%), C6/C7: 46 (27.5%), C3/C4: 16 9,6%), C7/T1: 2 (1.2%), C2/C3: 0 (0.0%)).
All surgeries were performed by four surgeons (BB (51 procedures, 85%), GR, DB, FK) following the same surgical technique. Anticoagulation and antibiotics were given to all 60 patients during surgery. The surgical approach in all patients is ventral from the right side. Mildly osteoporotic bone quality was observed in three patients (5%) during operation, 18 patients exhibited mild sclerosis, two patients a severe sclerosis, all other patients exhibited normal bone quality. The posterior longitudinal ligament (PLL) was partially resected for two patients, and complete removal was executed for the remaining patients, allowing visualisation of the ventral aspect of the dura. Partial resection of the uncovertebral process (foraminotomy) was done for two cases, an enlargement of the implant bed was done once. Additional measures were implemented in ten cases, one ablation of ventral osteophytes alone, one in combination with corpectomy of C5, three singular corpectomies (one at C5, twice at C6). One haematoma (ex domo pre-operation) was removed with subsequent fusion of C4 to C6, with explantation of the cage. In one case the cage size had to be corrected to one size up, and a second plate osteosynthesis was performed. In one case a revision cage was implanted with concomitant plate osteosynthesis. Cages implanted were Fidji cages in 59 cases, and in one case an Aesculap CeSpace cage was used. The plates used varied between 24 mm (one segment) and 103 mm (six segments, this was the plate used for the five-level patient, as the segments were higher and could not be treated with a five-segment plate). The most frequent plate implants used were two and three-segment plates, with lengths between 43 and 67 mm. In one case two plates were used.
In total 285 screws were used, all with 4 mm diameter, in lengths between 14 and 18 mm, with 16 mm being the most frequent length (14 mm: 31(10.9%), 16 mm: 248 (87.0%), 18 mm: 6 (2.1%)).
The surgical time ranged from 56 to 259 minutes, with an average of 123 minutes (STD 43 minutes). Blood loss was less than 100 ml in three cases (5%), between 100 and 500 ml in 41 cases (68%), and between 500 and 1000 ml in 16 cases (27%).
All 60 patients reported their outcome at the follow-up time-point. The average follow-up time was 2.9 years (standard deviation: 1.2 years). Clinical endpoints assessed were pain (VAS), function (NDI), dysphagia for liquids and solids (Bazaz index) and quality of life (European Quality Index in 5 dimensions, EQ 5D). Current neck and arm pain was recorded for left and right side, and at rest and under load. Neck pain values are overall higher than arm pain, and under load the patients always experienced more pain than at rest. A detailed overview is given in Table 2.
The mean NDI after follow-up was 10.4 points (corresponds to 20.8%) of disability out of 50 points (min 0, max 40 (corresponds to 80%), STD: 9.15 (corresponds to 18.3%)). This corresponds to a mean category of “mild disability” (5-14 points, 10 – 28%). Out of the 60 patients, 21 experienced no disability, 20 mild disability, thirteen patients moderate, and five patients a severe disability. One patient had complete disability.
The patients’ swallowing capability was assessed via the Bazaz score. 88% of patients did not experience swallowing difficulties with liquids, 71% were symptom-free when considering solids. The rest of the patients reported rare (4, 6.7%), or occasional (3, 5%) difficulties with liquids. Regarding solid food a few patients reported rare (5, 8.3%), occasional (7, 11.7%, only for certain foods such as bread or meat) or frequent (5, 8.3%, with the majority of food).
The EQ-5D evaluation included all 60 patients. On average, patients experienced a quality of life of 0.91, between a minimum of 0.31 and a maximum of 1.
Thirty-nine patients reported no neurological deficits at the follow-up examination. Seventeen reported sensory, one patient motor function deficits. In three cases a combined sensory and motor function deficit was reported. Compared to the preoperative situation the neurological status was improved for 43 patients. Eleven patients considered the neurological result as “maintained” with regard to the preoperative situation. Six patients did not experience any deficits, neither pre- nor postoperatively. None of the patients reported a worsened situation.
Fifty-one patients did not need pain medication at follow-up. Eight patients took “Stage 1” medication, according to the WHO scale (non-opioid analgesics), and one patient took “Stage 2” (low-potency opioid analgesics and non-opioid analgesics). None of the patients reported a “Stage 3” medication (high-potency opioid analgesics and non-opioid analgesics) according to the WHO scale.
Twenty-five patients returned to normal working life at follow-up, and eight patients did not. Six patients have claims to retire due to the medical restriction, and 21 patients are regularly retired.
When asked about their retrospective view on the surgery, 56 patients opted for being operated again, three did not know if they want to be operated again, and one patient stated clearly that he would not go for the operation again.
The study team was asked to report every Adverse and Serious Adverse Event that occurred between the index surgery and the current follow-up of their cervical procedure. So each operation, hospital stay, or further moderate or serious health problem was meticulously documented, independent of its correlation with the cervical spine and the index surgery.
Forty eight Adverse Events were assessed in total, 44 were considered “Serious”. None of the Adverse and Serious Adverse Events correlated with the study product. In five cases, the Adverse Event was linked to the procedure: in three cases local pressure on the anatomic structures during surgical approach lead to postoperative complaints. One instance of postoperative bleeding from the surrounding muscles occurred. In one case, a scar formation was seen leading to postoperative dysphagia, in this case a pre-existing degeneration of the C3/C4 segment was not treated during index surgery.
The mean onset of the Adverse and Serious Adverse Events was 18 months and the duration was 30 days, on average. In five cases, the SAEs were documented as unsolved. The most frequent short description of the event was “pain” for various reasons. A more detailed description allowed further classification of the AEs: thirteen events involved lumbar spinal problems, eight were located at the cervical spine, seven patients developed a malignant neoplasm at any location, five patients had other orthopaedic Adverse Events, leading to hip and knee replacements and other treatments. There were three cases of inflammation, four neurologic (including one apoplexy), three visceral and two cardiovascular problems. One patient suffered from dyspnoea, one serious posture problem and a vascular bleeding.
Radiological Outcome
The average radiological follow-up time was 1.8 years. This is shorter than the clinical follow-up, as in many cases the standard one-year X-ray was already available. Further imaging analysis was performed in a few patients, three CTs and four MRIs.
Complete anterior bone bridging between the treated segments was seen in one patient. Radiological density was visible in 49 patients, compared to the immediate postoperative status. In ten patients no bone bridges nor densifications could be identified.
Absence of visible radiolucencies along the plate screws could be confirmed in 58 patients, while in two cases a mild radiolucency, less than 25%, was identified.
A radiological loosening of the plate screw structure was absent in 57 cases, but was found in three patients. Only individual screws were loosened in these patients, but not the complete structure.
Discussion
ACDF is the treatment of choice for symptomatic degeneration and various other indications of the cervical spine in patients when conservative treatments, such as medication or physiotherapy, have failed.25 It is used to decompress the cervical spinal cord and the nerve roots in cases of herniated intervertebral disc, cervical radiculopathy, spondylosis, myelopathy or deformity caused by trauma, tumour or infection.26 Although ACDF is considered a safe procedure and its complications are relatively rare and manageable, some complications may be serious and could last for several weeks to months, or may lead to complete disability.27
Supporting implants used to perform an ACDF are various, from stand-alone cages to rigid and dynamic plates, plate and cage in one implant, or posterior cervical fixation.11,28 So far none of the methods has been found superior to all other options. But there is some evidence that the dynamic plate is slightly superior to a rigid design of the same geometry.19 In a biomechanical setup it was demonstrated that dynamic plating yielded no significant change at the C6/C7 but a 21% decrease in load at C4/C5 when compared with rigid plating, although the difference was not significant. Therefore dynamic plating may diminish superior adjacent level compressive stresses.
We present a prospective study on the dynamic version of the successor plate used by Pitzen.11 We re-examined patients who received ACDF in the past with this third generation dynamic cervical plate, and collected clinical and radiological data. Clinical outcomes were comparable to the literature and specifically with the studies reported by Pitzen, with overall minor disabilities for most of the patients after a mean of almost three years follow-up.11 On average, the examined subjects reported a low grade of NDI disability of 20.8%, corresponding to the category “mild disability”.22 Publications with similar products show comparable results for dynamic plating, although the average number of treated segments in this study was relatively high (2.8) and previously operated and revision patients were not excluded.
The retrospective view on the operation was overall positive; 93.3% patients confirmed that they would undergo the surgery again. This corresponds to quite high patient satisfaction when compared to the literature on ACDF.29
Design, shape, size, surface architecture of a cervical plate as well as bone quality and density need to be considered as important factors that influence the clinical and radiological results of cervical fusion.27 A significant proportion of patients show good recovery after ACDF, which was the case for the patients examined here. Our study has again demonstrated that ACDF is an effective treatment, significantly restoring quality of life to many patients.
Further research is necessary to elaborate a potential clinical benefit of the cervical plate investigated here, as mentioned in the biomechanical study, and as suggested by clinical and radiological studies.11,19 This could be in a randomised study setting that allows a direct comparison of this relatively new dynamic cervical plate design to its rigid counterpart. Other treatment options could be studied. For example a direct comparison with a disc prosthesis could be interesting as both concepts provide different levels of mobility to the treated segment, although they are based on completely different mechanical concepts. Here the inclusion criteria should be very strict in order to compare very similar indications.
Conclusion
Our study results revealed that the dynamic cervical plating combined with a cage is associated with good clinical results in the mid-term.
Acknowledgement
The authors would like to thank Nina Schröder for her support to organise the study in the hospital, identifying, finding and contacting patients, and resolving all patient issues during their examination in the hospital. She also supported completing the documentation.
Authors’ contributions, e.g., information about the contributions of both authors
Bernhard Bruchmann has contributed as follows:
-
BB contributed substantially to the conception and design of the work; he acquired, analysed, and interpretated the data for the work;
-
He drafted the work.
-
He gave the final approval of the manuscript version to be published.
-
He agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Francis Kilian has contributed as follows:
-
FK gave additional advice to the conception and design of the work;
-
He revised critically the important intellectual content;
-
He gave final approval of the manuscript version to be published.
-
He gave agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures about potential conflict of interests
Bernhard Bruchmann and Francis Kilian declare that they do not have any conflicts of interest.
Further information
The study was supported financially by Aesculap AG, Tuttlingen, Germany.


_preoperatively__b)_directly_postoperatively__and.png)
_preoperatively__b)_directly_postoperatively__and.png)