Introduction
Major orthopaedic surgery, especially hip and knee arthroplasties result in significant peri-operative bleeding and the need for allogeneic red blood cell (RBC) transfusion. Since pre-operative Hb concentration is a major predictor of peri-operative transfusion, haemoglobin optimization before surgery is a cornerstone in patient blood management (PBM).1 Intravenous (IV) iron is an essential drug to optimise pre-operative Hb concentration and consequently reduces anaemia and transfusion in patients with ID anaemia.2
Significant interest that healthcare institutions currently show for the PBM programme has a solid economic background since blood transfusion is one of the most abused and expensive treatments. Data from National Blood Centre (CNS) report decreasing rates of blood donors in Italy.3 Moreover, the population mean age is increasing meaning that in the future there will be a greater need for blood components for the elderly to a reduced pool of donors among young people. Finally, blood components quality and safety requirements are nowadays higher thus also increasing their cost.3 The multimodal PBM approach is more effective from both a clinical (see literature review before) and an economic4 point of view than the traditional transfusion approach. Nevertheless, the cost-effectiveness of Hb optimisation as a single PBM strategy has not been evaluated in patients undergoing orthopaedic surgery.
This study was aimed at evaluating the Hb levels at pre-hospitalisation, before and after surgery (day 1, day 3) and the cost-effectiveness of pre-operative Hb optimisation to avoid the need for RBC transfusion in JW patients undergoing TKA and refusing allogeneic blood.
Materials and Methods
Patients and study design
We conducted a retrospective study of 18 patients (11 females, 7 males) whom each underwent a TKA between January 2018 and October 2019. The preoperative diagnosis was knee osteoarthritis with an indication of primary arthroplasty. Two different groups were identified. Patients in both groups were generally well-matched and no significant differences were observed between groups regarding comorbidities (ASA, obesity, arterial hypertension, dyslipidaemia, diabetes, cardiopathy, BPCO, arrhythmias, osteoporosis, Crohn disease, thyroidectomy, CKD).
Group 1 included JW patients who refused blood transfusions and underwent a pre-operative Hb optimisation programme to avoid severe postoperative anaemia and subsequent transfusion indication. The preoperative Hb optimization programme started at least 1 month before the surgery programmed date. As anaemia (Hb concentration <13 g/dl in males and <12 g/dl in females) is a contraindication for elective surgery, 3 patients employed more than 1 month to obtain an indication for surgery. All Group-1 patients (with or without anaemia) underwent at least 1 Transfusion Medicine specialist’s consultation after pre-hospitalisation that, if necessary, prescribed one among these treatments: oral iron therapy (Ferrograd®, Sideral ForteV), IV ferric gluconate (Ferlixit®), IV ferric carboxymaltose (Ferinject® 500 mg or 1000mg); vitamin B12 (Dobetin® 5000 mg), oral folate (Folina® 5 mg, Lederfolin® 7,5 mg), EPO 20000 U.I., 30000 U.I., 40000 U.I (Binocrit®, Eprex®), intraoperative blood saving (IOS). Routine lab tests (HCT, Hb, MCV, RDW, MCH, MCHC) were performed and, when necessary to investigate the underlying cause of anaemia serum ferritin, serum transferrin, TSAT, folate, B12 vitamin. Further Transfusion Medicine specialists’ consultations were required to re-evaluate anaemia until no surgery contraindication was finally declared.
Group 2 included non-JW patients consenting to transfusion in case of necessity after surgery. They were not submitted to Transfusion Medicine specialist’s consultation nor erythropoietic stimulating therapy unless anaemia was diagnosed during the first pre-hospitalisation visit after lab tests. All Group-2 patients received RBC transfusion to correct postoperative anaemia according to local hospital guidelines (perioperative anaemia; Hb between 7-10 g/dL; age).
Drug prices were gathered from the AIFA website, while the cost of a single hospital transfusion medicine consultation was gathered from the regional price list.5 Two different price values were taken into consideration for RBC transfusion: € 181,00 is the price of a single RBC unit (as it was established by laws5) while the estimated cost of the entire transfusion procedures (blood group tests, type and screen, medical consultation, distribution procedures of blood components, traceability, hemovigilance, adverse reactions management) is € 400,00 according to CNS orthopaedic recommendations.3
Procedure
Surgical procedures were performed by two surgeons in both groups with identical operative techniques for primary TKA. Pharmacological antithromboembolic prophylaxis was administered in both groups: low molecular weight heparin (Clexane® 40000 UI) at a dose of 0.4 ml per day subcutaneously, starting from the evening before the operation and continuing for an average of 30 days. In both groups, TXA protocol was employed: IV 2 gr in 250 mL Phys. sol. 1h before surgery, 1 gr intra-articular injection with closed capsule, IV 2 gr in 250 mL Phys. sol. 3h after surgery. Esmarch bandage was applied and a pneumatic tourniquet was inflated before making skin incision and was used during all the steps of the procedure; it was released after wound closure and elastic dressing. No postoperative intraarticular drainage has been used, since there are no significant advantages regarding (in terms of) blood loss, transfusion rate and pain, meaning also cost saving.6
Statistical analysis
Results are expressed as the mean ± SD. The student’s t-test was used to perform pairwise comparisons for pre-hospitalisation, preoperative, day 1, day 2 and day 3 Hb mean values between the 2 groups. Wilcoxon rank-sum test was used to perform pairwise comparisons between Group-1 and Group-2 costs. Significance was set for p-values < 0.05.
Results
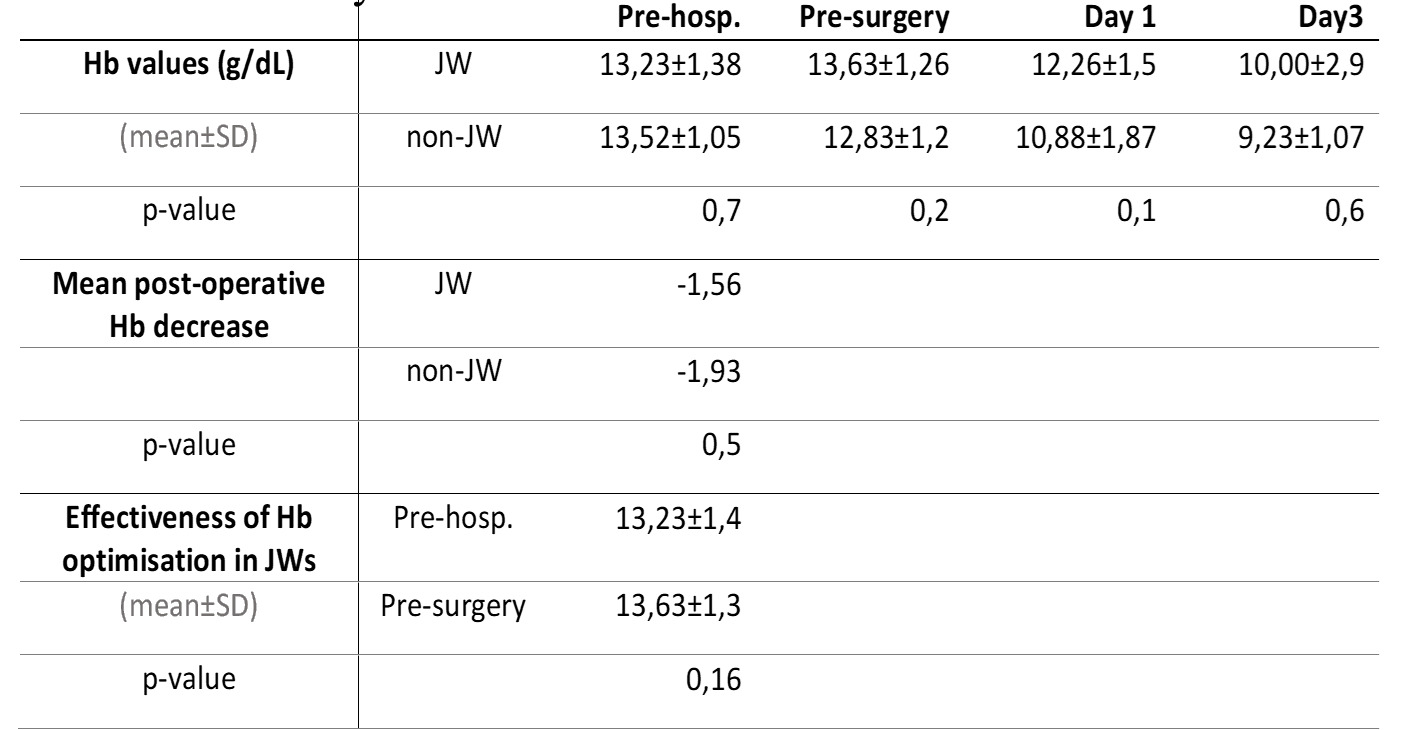
In the JW group (group 1) every patient was screened for preoperative anaemia detection and management, 3 patients were anaemic (33%), 7 anaemia was mild, received anyway no contraindication to surgery; the Hb optimisation programme seemed to be also effective in other non-anaemic patients, as they had better preoperative Hb. However, the effectiveness of the Hb optimisation programme in the JW group couldn’t be proved since there was no difference between after-treatment mean preoperative Hb (13,63±1,26 g/dL) and pre-hospitalisation (Hb 13,23±1,38 g/dL) (p=0,16). In the non-JW group (group 2) anaemia studies were not part of the standard of care and no patient received preoperative anaemia optimisation. 2 total patients (22%) were anaemic preoperatively (Hb<12 g/dL for the female sex, Hb<13 g/dL for male sex) in this group. They were all transfused after surgery since they all developed post-operative anaemia, while in the JW group only 3 patients developed postoperative anaemia 1 of which already entered surgery with non-responsive mild anaemia and remained mild anaemic also after surgery. There was no statistically-significative difference between patients who underwent perioperative Hb optimisation (JW group) and the non-JW group. Comparison between the 2 groups shows (Tab. 1): Hb levels before surgery (JW 13,63±1,26 vs. non-JW 12,83±1,21, p-value=0,22), after surgery (day 1 Hb: JW 12,26±1,47 vs. non-JW 10,88±1,87, p-value=0,1; day 3 Hb: JW 10±2,97 vs. non-JW 9,23±1,07 p-value=0,64). Hb concentrations declined following surgery. In the JW group the mean Hb concentration decreased from 13,63±1,26 g/dL preoperatively to 12,26±1,47 g/dL (day 1). In non-JW group the mean Hb concentration fell from 12,83± g/dL preoperatively to 10,88± g/dL (day 1). There was no difference in the magnitude of the mean operative decrease in Hb concentration between the JW group and the non-JW group (-1,56 g/dL vs. -1,93 g/dL respectively, p-value=0,51) (Fig. 1).
Cost-wise, total expenses to treat the JW group (including drugs and transfusion medicine consultations) were 5070,68 € (Fig. 3), while the non-JW group cost 2896,00 € considering only the price of an RBC unit (JW patient mean cost 563,41 € vs. non-JW patient mean cost 321,78 €) (Fig. 2). However, taking into consideration the cost of the entire transfusion procedures (blood group tests, type and screen, medical consultation, distribution procedures of blood components, traceability, hemovigilance, adverse reactions management) the situation is reversed since the cost of the non-JW group rises to 6400,00 € (JW patient mean cost 563,41€ vs. non-JW patient mean cost 711,11 €) (Fig. 2). Anyway, in both cases the mean cost of the 2 groups has no statistically-significative difference (p>0,05), meaning that from a statistical point of view the two groups of treatment have the same economic burden.
Discussion
We performed a retrospective study evaluating the effectiveness of a change of practice of preoperative treatment of anaemia utilising iron supplementation as recommended by CNS orthopaedic recommendations3 to reduce the rate of allogeneic blood transfusions. This new approach testing took place firstly in JW patients who refuse blood transfusions for religious reasons, considering their bloodless-surgery approach an opportunity to implement blood-saving strategies whose benefits will affect every patient. Previous studies proved that preoperative Hb optimisation programme reduced the incidence of postoperative anaemia and the use of allogenic blood transfusion in TKA.7 Hou et al. found that Hb level at admission <12.4 g/dL is a predictor of blood transfusion8 thus, a good optimisation programme can permit to perform this type of surgery safely. This is confirmed by another study showing that a good preoperative Hb protocol allows executing joint arthroplasties without allogeneic transfusion in anaemic patients.9 In addition, this is in accordance with a recent review on JW by Mottla et al. which stated that with a preoperative optimization programme, arthroplasties are safe.10 Moreover, RBCs transfusion have several adverse effects identified in different studies. These comprise longer hospital stays, increased 90-day mortality, post-operative cardiac complications, acute haemolytic reactions, pneumonia and bacterial infections.11–13 We compared this approach (JW group) to the transfusion-based approach without preoperative Hb optimisation (non-JW group), proving that JW patients have better Hb values pre and post-operatively. We compared this approach (JW group) to the transfusion-based approach without preoperative Hb optimisation (non-JW group). No significant difference was shown among pre and post-operatory (day 1, day 3) Hb values of JW patients and non-JW patients (p>0,05). This was probably caused by the low numbers of patients (n=9) considered in each group of this study. Other studies showed higher Hb values postoperatively in the patient who underwent perioperative Hb optimisation.7 A similar study that we conducted in patients undergoing THA showed the statistically-significative difference between Hb values in 10 JW patients who underwent Hb optimisation preoperatively than in the control group. We also analysed the costs of these 2 approaches, since the PBM approach is more effective from an economic point of view than the traditional transfusion approach,4 but the cost-effectiveness of Hb optimisation as a single PBM strategy has not been evaluated in patients undergoing orthopaedic surgery so far. We found that, despite the great number of expensive drugs, lab tests and transfusion medicine consultations, there is no significant difference (p>0,05) between the mean cost of Hb optimisation in a JW patient and the mean cost for transfusions in non-JW patients. Costs directly borne by our clinic may seem greater for a Hb optimisation programme than a blood-transfusion approach, but considering the overall esteemed cost of the whole transfusion procedures for the SSN (€ 400,00),3 the PBM approach reveals its economic convenience. We should also consider savings of blood components, given decreasing rates of blood donors and increasing blood components costs because of more strict safety requirements. This point of view was not considered in our study, since all non-JW patients received a blood transfusion, but it is proved by other studies.7 Furthermore, several studies on restrictive haemoglobin transfusion threshold showed the same or better perioperative outcomes compared with a more liberal transfusion threshold.14 This is also confirmed by Gupta et al. which demonstrated how restrictive haemoglobin policy, combined with good patient blood management is well tolerated even in elderly patients.1 Other studies analysed the cost-effectiveness of preoperative Hb optimisation strategies and they also found seemingly increased costs in the optimisation group.15 A hypothetical computer-simulated trial study calculated the cost per transfused patient avoided and RBC unit spared for the different probability of transfusion in the optimisation group. As expected, costs increased exponentially as the probability of transfusion decreased. There were no differences in transfusion requirements between the optimisation and control group for probabilities of transfusion over 20%. Cost savings fall to zero when the proportion of patients who would require transfusion in the optimisation arm decreases. In other words, Hb optimisation is disadvantageous when applied to patients with low transfusion probabilities, while it is economically advantageous when applied to patients with high transfusion risk. The limit of this study is that we applied the Hb optimisation programme to all group 1 patients since they were JW refusing blood transfusion in any case, also when of vital necessity, so we had to eliminate every risk of recurring to blood transfusion.
Conclusions
PBM programs offer different treatment strategies to face Hb optimization in elective surgery. Our study adds to the growing body of literature regarding the efficacy of PBM that can be applied not only in JW patients. It represents a safe strategy, reducing the risks and costs and improving outcomes. Not less important, it permits to reduce transfusion overuse.
Conflict of interest
The authors declare no conflicts of interest.
Funding
None.


__group_2_(transfused__single_rbc_unit_cost)__group_.png)


__group_2_(transfused__single_rbc_unit_cost)__group_.png)
