INTRODUCTION
Periprosthetic fractures after total knee arthroplasty are a rare traumatic lesions but their incidence have increased recently due to the ever higher number of total knee replacement implanted worldwide.1 The most common periprosthetic fracture after total knee arthroplasty affects the distal part of the femur, with an incidence ranging from 0,3% to 2,5% of all patients operated on for primary knee replacement,2–4 however this percentage increases until 38% in revision arthroplasty.5 In a recent study, other authors report a higher incidence of these lesions, reaching 5.5% and 30% after primary and revision arthroplasty respectively.6 These fractures are often difficult to treat due to the elderly age of the patients often affected by osteoporosis and presence of multiple comorbidities such as metabolic disorders, hypertension, heart diseases, vascular diseases etc.2,7–11 The most widely used classification of distal femoral periprosthetic fractures was reported by Rorabeck and Taylor that described three different types: type I, in which a non-displaced fracture is present with intact femoral component; type II, in which the fracture is displaced but the femoral component is stable; type III in which the fracture is associated to a femoral component loosening.12 The most commonly used method for the treatment of periprosthetic distal femoral fractures is open reduction and internal fixation (ORIF) with locked plating or retrograde intramedullary nailing; revision arthroplasty is indicated only when the fracture is located at the very distal part of the femur or when the loosening implant is present (type III). Regarding the method of internal fixation, comparative studies between the use of locked plating and intramedullary nailing are quite rare, therefore the “standard method” of treatment of these lesions is still debated.13–17
In the present study, we report the medium to long-term results in 12 patients affected by periprosthetic femoral fracutures type II according to Rorabeck and Taylor classification, surgically treated by open reduction and internal fixation using a locking plate.
MATERIAL AND METHODS
We selected 12 patients with a periprosthetic distal femoral fracture after total knee arthroplasty treated in our institution between 2012 and 2016 by open reduction and internal fixation (ORIF) with locking plate. Two were male and ten female with a mean age of 78 years (from 53 to 92). All patients had an appropriate clinical and radiographic documentation and were analysed retrospectively after a mean follow-up of 5.75 years (from 3 to 11 years). Ten patients had a primary total knee arthroplasty and two a revision arthroplasty; all implants were cemented. In all patients, the periprosthetic distal femoral fracture occurred after a low-energy trauma, however in 9 of them some predisposing factors were present: 2 patients with rheumatoid arthritis were chronic steroid users; 3 patients had diabetes mellitus and 4 patients were obese. Total knee replacement had been performed for osteoarthritis in 10 patients and for rheumatoid arthritis in 2. Both the patients affected by rheumatoid arthritis underwent primary total knee arthroplasty. The mean interval time between knee arthroplasty and periprosthetic distal femoral fracture was 8.25 years (from 2 to 15 years). All patients were treated by ORIF using a locking plate fixed by screws. After surgery, postoperative radiographs were performed to assess the quality of the reduction and all patients started the physical rehabilitation immediately after surgery, with progressive weight bearing after 4 weeks. Clinical and radiographic examinations were performed after 1, 3 and 6 months after surgical procedure. Regarding the bone quality status, no patients were investigated after surgery but all of them were sent to the osteoporosis clinic one month later, at the first follow-up.
The study has been approved by the Ethical Committee of our Hospital - Policlinico di Tor Vergata, Rome, Italy. Oral informed consent was obtained from all partecipants.
STATISTICAL ANALYSIS
Statistical analysis was performed to find possible correlation between the following variables as sex, implant indication (osteoarthritis or rheumatoid arthritis) and interval between implant and distal femoral fracture with clinical result at follow up evaluated according to WOMAC score. Statistical analysis was also performed to find possible correlation between clinical and radiographic results at follow-up, evaluated according to Beals and Tower criteria.
The Student’s t-test and Mann-Whitney U test were used to evaluate the significance of differences for continuous variables. All statistical analyses were performed using the SigmaStat Version 4.0 program (Systat Software, Inpixon, CA, USA); p-values lower than 0.05 were considered significant.
RESULTS
At last follow-up, clinical results were assessed according to the Western Ontario and McMaster Universities osteoarthritis index criteria (WOMAC) that provides for a total score ranged from 0 (best result) to 96 (worst result). The WOMAC measures five items for pain (score range 0-20), two items for stiffness (score range 0-8), and 17 for functional limitation (score range 0-68). Higher scores indicate worse pain, stiffness and functional limitations.18
Radiographic results were assessed according to the Beals and Tower’s criteria19; final result is considered excellent when the arthroplasty was stable and the fracture healed with minimal deformity without shortening; it is considered good, when there was a stable subsidence of the prosthesis or when the fracture healed with moderate deformity or shortening, while it is considered poor when there was a prosthesis loosening or painful, non-union, sepsis, new fracture, severe deformity or severe shortening.
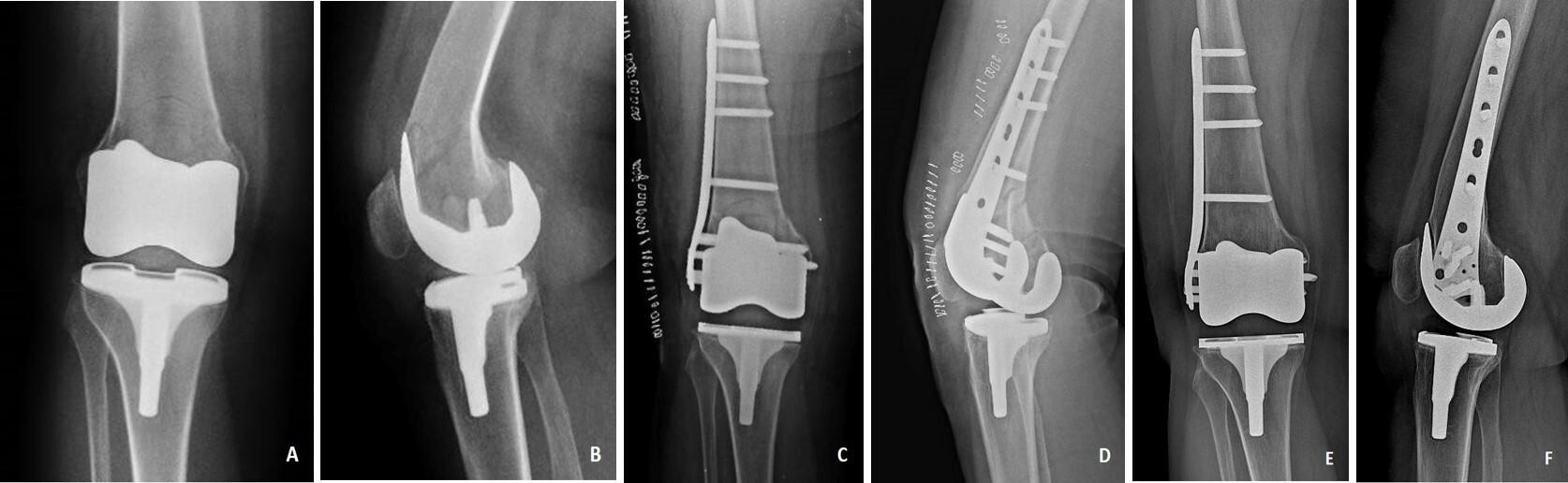
Demographic, clinical and radiological results of our patients are reported in Table 1. According to Rorabeck and Taylor classification, all fractures of our series were type II (displaced fracture without loosening of the femoral component). At final follow-up, the mean value of WOMAC score was 53.92 points (from 40.5 to 76.5). Radiographic results, according Beals and Tower’s criteria, were excellent in 5 patients and good in 7. No patient had a poor radiographic result. All patients were satisfied with the final result and returned to their previous daily activities (Fig. 1, 2).
There were no statistically significant correlations between sex, implant indication, interval between implant and fracture and WOMAC score (p > 0.05). Similarly, there was no statistically significant correlation between WOMAC score and radiographic results (p > 0.05).
DISCUSSION
Periprosthetic fractures of the distal femur may be difficult to treat due to numerous risk factors of the patients, such as elderly age, poor bone stock and various comorbidities often present.6,10–23 The most widely used classification of these fractures was described by Rorabeck and Taylor that emphasizes two variables, displacement of the fracture and the stability of femoral component of the knee prosthesis.12 The most common periprosthetic fracture of the distal femur is Rorabeck type II in which a displaced fracture is associated to a stable prosthesis. These data are in agreement with our series of patients, in which all fractures were classified as Rorabeck type II. The management of these traumatic lesions may be different. Conservative treatment by cast or brace application should be used only in patients with a high risk of perioperative complications.1 Surgical management represents generally the treatment of choice, but the method of fixation after reduction is still debated. The two most common procedure are locking plate fixation or retrograde intramedullary nailing but in selected cases an external fixation or a revision arthroplasty may be performed, especially in very distal femoral fractures. Rorabeck II fractures may be indifferently stabilized after reduction using plate and screws or retrograde nail; however in some cases the type of femoral component of knee prosthesis does not allow the introduction of the nail, therefore in these cases the use of a plate is mandatory.
Ebraheim et al4 in a systematic review on periprosthetic distal femoral fractures after total knee arthroplasty analyzed a total of 448 fractures and reported that the two most successful treatment options to stabilize these lesions were locking plate and intramedullary nail/rod with similar healing rates. However, the complication rate in the locked plating series was lower than in intramedullary nailing. Shah et al17 in another systematic review reported that both locking plate fixation and intramedullary nailing offer analogous benefits for treatment of these lesions but concluded that the advantages and disadvantages of both treatment options remain controversial. Tosounidis and Giannoudis6 in their study confirmed that in distal femur periprosthetic fracture the main internal fixation techniques are lateral locking plating and retrograde intramedullary nailing. They suggest in some cases to use a supplementary medial plate and recommend the nailing in the fractures located above the anterior part of the femoral component of the implant. Benkovich et al1 in a comprehensive review report that it is not uncommon that the surgeon decides the operative method of fixation in the operating room, choosing between locking compression plate and intramedullary nailing. Nagwadia and Joshi24 in a retrospective study reported promising results in 29 patients with a Rorabeck type II fracture treated with a locking compression plate.
Darrith et al25 compared ORIF to distal femoral replacement (DFR) in a series of 72 patients affected by a displaced periprosthetic distal femoral fractures; 50 patients were treated with ORIF and 22 with DFR. The authors concluded that the KSS score (Knee Society Score)26 favored ORIF but the total incidence of revision was higher in the ORIF cohort. Lex et al11 in a recent systematic review concluded that DFR is more reliable in complex fractures if an adequate fixation is hard to achieve.
In our series all fractures were Rorabeck type II and they were treated by open reduction and internal fixation with a lateral locking plate. No patients needed a supplementary medial plate. At final follow-up, we observed excellent or good radiological results in all patients although the WOMAC score was not always satisfactory. However, all patients were satisfied with the final result and returned to their previous daily activities.
The main limitations of our study are that it is retrospective, without any control group and the number of cases is quite limited.
CONCLUSIONS
In conclusion we believe, in agreement with other authors,4,24,25,27 that in Rorabeck type II periprosthetic distal femoral fractures, open reduction and internal fixation with a locking plate is a surgical option of treatment that provides satisfactory clinical and radiological results.