Introduction
Reverse total shoulder arthroplasty (RTSA) was first described in 1979 by Baylay and Kessel et al., and the Grammont style was developed in the last century.1–3 The first indications for RTSA were rheumatoid arthritis and tears of the rotator cuff. Eventually, the design and surgical technique for RTSA have been constantly developed, and the indications clearly broadened. Good clinical results have been achieved with RTSA.4 Due to the broadening indications for RTSA and the increasing rates of patients undergoing RTSA, complication rates have also increased,5 with reported complication rates of 10%–41%.6–12 The most common complications are impingement, scapular notching, instability, infection, aseptic loosening, and periprosthetic fractures.13–16 Periprosthetic fractures are often stress fractures at the acromion and scapular spine, with an incidence between 3.1% and 10%.5 The risk factors for postoperative acromion fractures are diverse. Werthel et al., who examined a total of 1,082 shoulders after an RTSA, observed an association of these fractures with osteoporosis, smaller lateral humeral offset, greater arm lengthening, and thinner acromion.17,18 Zmistowski et al. found that female patients with increased center-of-rotation medialization were predictors of postoperative acromion fractures in a total of 1,170 shoulders with RTSA.19 Acromion fractures were theorized to be caused by excessive tensioning of the deltoid muscle with additional weakening of the junction between the scapular spine and the scapular body caused by the drill holes in the metaglene.17,20–22 Furthermore, prosthesis design has been described as a risk factor for these fractures.23,24 The clinical results of patients with an acromion fracture after RTSA were inferior to those of patients without an acromion fracture.5 In addition, the clinical results before and after the development of acromion fracture were worse in the same patients.25 Treatment for acromion fractures is controversial. Crosby et al., who classified acromion fractures into three distinct patterns, proposed that type I fractures should be treated conservatively.20 Conversely, type II and III fractures were declared to be unstable and required open reduction and internal fixation.20 Levy et al. reclassified acromion fractures and recommended conservative therapy regardless of the fracture type.23,26 Conservative therapy involves the use of an abduction splint to reduce pain and decrease the deltoid traction on the fracture line for 6 weeks.24 Despite immobilization, a high rate of bony non-union of up to 66% has been reported.5,22,27 For the operative therapy, open reduction and internal fixation are described.20,27 This is challenging due to the mechanical force of the deltoid muscle and an often osteoporotic bone.24 There are no superior clinical results for operative therapy.5,24 Kicinski et al., who performed a biomechanical study comparing three plates for a type III acromion fracture according to Levy et al.'s classification,26 observed that the locking compression plate had superior biomechanical properties compared to a lateral clavicular plate or reconstruction plate.28 Further, superior results were observed for a double-plate configuration in osteoporotic fractures.29 Based on this and the standard clinical procedure for a double-plate osteosynthesis of dislocated acromion fractures, this biomechanical study aimed to investigate the biomechanical properties of a double-plate osteosynthesis compared to that of a single-plate osteosynthesis for acromion fractures. Our hypothesis is that double-plate osteosynthesis will show superior biomechanical properties with regard to primary stability than that of single-plate osteosynthesis.
Methods and Methods
Ethics approval
The ethics committee approved this study (8714_BO_K_2019). All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or with comparable ethical standards.
Specimens
For this study, 16 fresh frozen human cadaveric scapulae (Science Care Inc., Phoenix, AZ, USA) were used. There were 6 right and 10 left scapulae. The mean age was 61.3 years (standard deviation [SD] 9.7), and the mean body mass index was 24.4 kg/m2 (SD 4.4). Eight donors were men, and eight were women. Macroscopically, no previous surgical procedures have been observed or documented in their medical history. Further, no macroscopic differences were seen in bone quality or texture between the specimens. The age, weight and body-mass-index were not different between the two groups. Only the height showed a significant difference (p= 0.045) between the two groups.
Specimen preparation
The human cadaveric scapulae were thawed to room temperature and completely freed from soft tissue. The lower part was embedded in cold curing casting resin (RenCast® FC 52/53 Isocyanate, FC 53 Polyol, and Füller DT 982, Gößl & Pfaff GmbH, Karlskron/Braunlach, Germany) using a custom-made box. During the surgery and biomechanical testing, the specimens were soaked with 0.9% NaCl (Fig. 3).
Surgical technique
All surgeries were performed by a senior author. A type III acromion fracture according to Levy et al.'s classification was made with a saw. After fracture simulation, the specimens were randomized into two groups. In the first group, single-plate osteosynthesis using a locking plate was performed. Therefore, an eight-hole 3.5-mm locking compression plate (Depuy Synthes, Raynham, MA, USA) was used. The plate was adapted to the curvature of the scapular spine/acromion and placed on top of it. Always three screw holes, each medial and lateral to the fracture, were filled with locking screws after length measurement. The screws were tightened with an appropriate torque wrench (Fig. 1). In the second group, double-plate osteosynthesis was performed. The first plate was placed and fixed in the same manner as the single plate in the first group. The second plate was placed inferiorly from the scapular spine and perpendicular to the first plate. The second plate was a 3.5-mm one-third tubular locking plate (Depuy Synthes, Raynham, MA, USA). After drilling, three screws were placed medial and lateral to the fracture. The screws were tightened with a torque wrench (Fig. 2).
Testing protocol
The testing protocol was performed according to Kicinski et al.28 Each specimen was placed in a material testing machine (MTS 858 Mini Bionix®, Eden Prairie, MN, USA). The specimens were mounted in a material testing machine so that the embedded part was facing the floor. A 2.5-kN low-force load cell was used (FR10M-2.5KN-wB007, Tovey Engineering Inc., Phoenix, AZ, USA). To simulate the physiological force of the deltoid muscle, which directly influenced the acromion stress, a custom-made device attachment was produced, which had no contact with the plates. Force was directly applied on the superior surface of the acromion (Fig.3). The preloading force was set at 30 N. This protocol was similar to that of Kicinski et al.28 The failure of the osteosynthesis was defined as abrupt loss of load, and the material testing machine was stopped. The modes of failure were also documented.
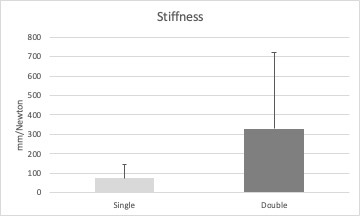
During biomechanical testing, the stiffness and translation were measured with an optical tracking system (Optotrak Certus, NDI, Waterloo, Canada), that is, the resulting three-dimensional translation of the acromion relative to the scapular spine. The 3D accuracy of the optical tracking system was 0.1 mm, and the resolution was 0.01 mm. Optical tracking markers were placed on the acromion and the other on the scapular spine. The three-dimensional coordinate system of the optical measurement was defined by tracking four bony landmarks (acromial angle, trigonum scapulae, superior glenoid, and inferior glenoid). The coordinate system was defined with the x-axis pointing inferior (superior glenoid to inferior glenoid), the z-axis pointing lateral (trigonum scapulae to acromial angle), and the y-axis perpendicular to the x-z plane pointing anterior. The origin was placed on the acromial angle. Because the angulus inferior was not accessible, the coordinate system was adapted to the recommendations of the ISB30(p200) (Fig. 3). The stiffness was defined as force per distance (N/mm).
Statistical analysis
Statistical analysis was performed using SPSS 25.0 for Windows (SPSS Science Inc., Chicago, IL, USA). Randomization was performed before conducting the surgical technique. Owing to the small number of specimens, calculation of the normal distribution was not necessary. To compare the two groups, the nonparametric Mann–Whitney U test for independent samples was used, and p-values < 0.05 were considered statistically significant. All data were presented as mean ± SD.
Results
The average load at failure was 167 N (SD 99.2) in the single-plate osteosynthesis group and 233.7 N (SD 127.7) in the double-plate osteosynthesis group. This difference was not statistically significant (P = 0.328) (Fig. 4). The average translation was 11.1 mm (SD 5.8) in the single-plate osteosynthesis group and 16.4 mm (SD 17.2) in the double-plate osteosynthesis group, but the difference was not significant (P = 0.753) (Fig. 5). The difference in stiffness between the two groups was 253.2. The mean stiffness was 74.7 N/mm (SD 69.2) in the single-plate osteosynthesis group and 327.9 N/mm (SD 394.3) in the double-plate osteosynthesis group, but the difference was not significant (P = 0.141) (Fig. 6). In the first group, the screws on the spina scapula broke out of the bone medial to the fracture in six cases and in one case lateral to the fracture. In one case the spina scapulae showed a splinter fracture. In the double-plate osteosynthesis group, the failure of the osteosynthesis with breaking out of screw medial to fracture in six cases. In one case the scapula showed fracture, which went to the spina scapula An acromion fracture was observed in one case.
Discussion
This study aimed to compare single-plate and double-plate osteosynthesis for acromion fractures as complications after RTSA and showed a tendency for superior biomechanical properties in those undergoing double-plate osteosynthesis, but this was not significant. According to Levy et al.'s classification,26 acromion fractures are postoperative complications of RTSA implantation, with an incidence between 0.9% and 7.2%.25 This RTSA complication has been underestimated, because these fractures are infrequent and difficult to diagnose. As evidenced by Otto et al., only 79% of these fractures were identified by blinded reviewers using plain radiographs alone.17 The therapy is controversially discussed in the current literature. Crosby et al., who classified these fractures, recommended conservative treatment for type I fractures, and patients did not undergo further intervention.20 For type II fractures, the authors discussed the influence of the AC joint and suggested resection of the AC joint for stable factures.20 Unstable fractures should be operated through open reduction and fixation.20 Type III factures may be caused by the superior screw of the metaglene. These fractures are often dislocated and should be operated on.20 Other authors recommended only conservative treatment regardless to the type of fractures.26 Due to the increasing number of patients undergoing RTSA, the number of complications can also be expected to rise, including acromion fractures. Based on the fracture location, both the middle and posterior parts of the deltoid can be affected, and dislocation of the fracture can lead to secondary impingement and decreased deltoid strength.29 This could be due to the inferior clinical results of patients with RTSA and acromion fracture.5,25 Teusink et al., who examined 25 patients with acromion fracture after an RTSA and 100 patients without a fracture in a case-control study, found inferior results in patients with fractures in the ASES and range of motion; however, fracture location and fracture healing had no effect on the outcome.25 Patients with periprosthetic fractures have a higher risk for surgical revision.25 In the systematic review, 3,838 patients after a RTSA were observed and 159 patients suffered from an acromion fracture.5 Only in 14% of these patients with an acromion fracture an internal fixation was performed5. Regardless of the therapy, patients with periprosthetic fracture had poorer clinical outcomes.5 In contrast, Toft et al. reported that five patients with a spina scapulae fractures after a RTSA, who were treated with a double-plate osteosynthesis, had similar clinical results after ORIF compared to the clinical results after RTSA and concluded that osteosynthesis is a valuable option in these patients.31 The osteosynthesis consisted of a locking compression plate and quarter tubular plate with 2.7 mm screws.31
Three other biomechanical studies evaluated osteosynthesis in those with acromion fractures after RTSA. Kicinski et al. investigated 19 Sawbones scapulae with three types of osteosynthesis for acromion fractures, and the locking compression plate showed the highest load at failure compared to that of the lateral clavicular plate or reconstruction plate.28 The load at failure was 506 N for the locking compression plate, 376 N for the lateral clavicular plate, and 360 N for the reconstruction plate.28 In 12 specimens with osteoporosis and 4 specimens without osteoporosis, Katthagen et al. observed that double-plate osteosynthesis achieved higher fixation strength in simulated fractures of the scapular spine in 12 specimens with osteoporotic bone.29 The mean load at failure was 471 N for the double-plate osteosynthesis and 328 N for the single-plate osteosynthesis.29 For the double-plate osteosynthesis, 3.5- and 2.7-mm locking compression plates were used. Our results supported partially the findings of Katthagen et al., because they also found no significant difference between single and double plate osteosynthesis in their complete collective. They used a 3.5 mm 6 holes locking compression plate (Depuy) and 2.7 mm 6 locking compression plate (Depuy). Another difference was the application of force on the acromion. Katthagen et al. applied force by attaching two sutures to the medial and posterior parts of the deltoid muscle at the acromion site, and these sutures were connected to the material testing machine.29 In contrast, the force in our study was directly applied to the acromion through stamping. Furthermore, bone density was not measured in the present study. The clearly higher loads at failure in Kicisnski et al.'s study could be explained by the use of Sawbones. In a study by Basso et al., who compared 10 composite femurs (Sawbones, Pacific Research Laboratories, Inc., Vashon, WA, USA) on 24 human cadaver femurs with subcapital femur fracture and screw fixation,32 the results showed a significantly lower head fragment migration in the group with composite femurs; therefore, the authors concluded that the composite femurs provide an unrealistic stable bone–implant construct and failed with different fractures compared to that of the cadaveric femurs.32 Ting et al. performed a biomechanical study with 24 fresh frozen cadaveric scapulae and compared a subcutaneous border plating and supraspinatus fossa plating with or without hook for simulated Levy type II fractures.33 The subcutaneous border plating with a lateral inferior supporting hook seemed to be advantageous for the internal fixation of type II scapular spine fractures after RTSA.33 These findings and the results of Katthagen et al.'s study support the hypothesis that an additional plate or hook provide more stability, but only for osteoporotic bone. In addition, the results of this study showed a higher load at failure in specimens with double-plate osteosynthesis, but this was not significant. The selected plate configuration may be reason why no greater stability with double plate osteosynthesis was achieved. The one-third tubular plate had a minor primary stability compared with a compression locking plate. Another difference to the study of Katthagen et al is that in this study longer plates were used and the holes next to fracture were left free. Katthagen et al positioned the plate that the fracture was directly between two holes of the plate. It is well known, that the use of screws in locking plate close to the fractures has the advantage of stable fixation, but due to the lack of swinging distance there is an increased stress on the locking plate. In contrast to Katthagen et al. in this study only locking screws were used, which also increased the stability of the osteosynthesis. This plate configuration was chosen in the study, because it was used in the everyday clinical practice and this application should be biomechanically test. Due to the limited space and good modeling properties, the tubular plate was chosen as the second plate. This is not sufficient in acromion fractures.
From a clinical point of view, double-plate osteosynthesis requires more operation time and produces higher material costs and a higher risk of infection; therefore, if there are no biomechanical advantages of double-plate osteosynthesis, it must be critically considered and is indicated for osteoporotic bone.
Our study had several limitations. First, it was a biomechanical in vitro study using human shoulder cadavers at time point zero; therefore, potential biological effects affecting the stability of the osteosynthesis, such as soft-tissue and bone healing, and muscle tension could not be investigated. Second, bone density was not investigated to determine the presence of osteoporosis in the specimens. Third, the application of the force was pointwise on the acromion, which differed from that in vivo.
Double-plate osteosynthesis using a one-third tubular locking plate and 3.5-mm locking plate provided the same primary stability compared to that of single-plate osteosynthesis using a 3.5-mm locking plate for acromion fractures after RTSA. The results suggested that the choice of plate configuration provides no superior results and that single-plate osteosynthesis is sufficient for acromion type III fractures.
Conflicting interests
MFP receives speaker fees from Depuy Synthes, TS is consultant of Depuy Synthes. DN, AD, RK, HH and AE declared to have no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or notfor-profit sectors.
Informed consent
Informed consent was not sought for the present study because it was a cadaveric study.
Ethical approval
Ethical approval for this study was obtained from ethics committee of the Medical School Hannover (8714_BO_K_2019).
Contributorship
MFP major contributor in writing the manuscript, data collecting, analyzed data and development of the protocol, DN performed and monitoring the biomechanical testing as, AD performed the biomechanical testing, RK and HH researched literature and analyzed the data. TS analzyed the data and corrected the manuscript as native speaker, AE wrote the manuscript, development of the protocol, analyzed data. All authors reviewed and edited the manuscript and approved the final version of the manuscript.