Introduction
Lower back pain (LBP) remains a significant global public health problem, affecting an estimated 7.5% of people worldwide.1 Among those suffering from LBP, more than half are found to have lumbar intervertebral disc pathologies, such as radiculopathy, spinal stenosis, and herniations.2 Lumbar disc herniations (LDH) are a common cause of LBP; affecting 2-3% of the general population and often requiring decompressive surgical interventions.3
The lumbar spine is composed of five vertebral bodies and intervertebral discs with spinal nerves exiting below their corresponding vertebrae. LDH is characterized by the displacement of the nucleus pulposus (NP) through the annulus fibrosus, leading to mechanical compression and chemical neuritis of the spinal nerve roots.4 Physical compression may promote thrombus formation and ischemia leading to increased pain sensitization while the release of proinflammatory chemokines chemically injure cells and facilitates neuritis.4,5 In both cases nerve fiber injury may be induced through intraneural edema which decreases neural conduction velocities.6
Understanding the connections between LDH and sciatica has led to the implementation of non-surgical and surgical treatment approaches for LDH. Intradiscal injections aim to treat the symptoms of sciatica while maintaining a minimally invasive approach.7–9 Surgical procedures attempt to increase the intervertebral space or resect the LDH to alleviate nerve compression.10 The breadth and scope of treatments for LDH have vastly evolved over the last few decades, from intradiscal therapies to open surgical laminectomies.11–14
Comprehension of the various approaches to LDH, cost of the procedures, antibiotic use, and recurrence after treatment is imperative in identifying indications and delineating the benefits and downsides of each treatment modality. There exist scattered reviews providing a comprehensive description of the surgical modalities of LDH as well as alternative intradiscal injections, peri- and post operative antibiotics, cost analysis of the procedures, and post-operative management of recurrence. This compilation review attempts to summarize our current understanding of all such fields. When appropriate, we note the adverse effects of treatment approaches and comment on the future direction of LDH management.
Methods
The present study was conducted as a comprehensive literature review using PubMed and Google Scholar. Articles relevant to summarize the previously mentioned topics of LDH management were reviewed. Then, at least two authors assessed and selected articles according to our inclusion and exclusion criteria (Table 1). A wide breadth of articles was reviewed in this study to provide a comprehensive narrative review of recent literature regarding treatments for LDH. Therefore, keywords and PRISMA guidelines were not utilized. However, the selected literature was scrutinized according to the GRADE (Grading of Recommendations Assessment, Development and Evaluation) guidelines and only studies that were level II evidence or higher were included. Gray literature, case series, case reports, and expert opinions were excluded from the study. There were no disagreements present among the authors for the chosen studies.
Results
Intradiscal Injections – a bridge between conservative and surgical approaches
Intradiscal injections are a minimally invasive option that consists of percutaneous injection to the nucleus pulposes and is typically guided by imagining such as real time-multiplaner fluoroscopy.15 Chemonucleolysis is the intradiscal injection of a proteolytic enzyme in the nucleus pulposes leading to chemical dissolution of herniated material.16 Chymopapain was previously utilized for chemonucleolysis and studies found it to effectively eliminate or reduce LDH associated pain. One review of 45 chymopapain studies involving 7,335 patients LDH from 1985 to 1993 reported a cohort clinical success rate of 76%.17 However, rare complications of anaphylaxis were observed partly due to the effect of its low substrate specificity on surrounding tissue.18,19 Despite its success chymopapain was withdrawn from commercial use in 2002 due to non-scientific commercial reasons.20
Chondroitin sulfate ABC endolyase (condoliase) is an alternative to chymopapain that was recently approved for use in 2018. It is a mucopolysaccharide-degrading lyase that targets chondroitin sulfate and hyaluronic acid glycosaminoglycans of proteoglycans present in the nucleus pulposes.21,22 Unlike chymopapain, damage to surrounding neural and vascular tissue is mitigated due to its high substrate specificity and lack of protease activity.23 Many recent studies support the efficacy and safety of a single 1.25 U/mL dose injection of condoliase in LDH patients. A phase III randomized control trial by Chiba et al.24 compared a single dose injection of 1.25 U/mL condoliase in 82 LDH patients to 81 patients with placebo. Significant reduction in volume of intervertebral disc and herniated mass, disc height, and worst leg pain scores at 13 weeks and one year were recorded without significant clinical consequences. Okada et al.,21 evaluated 82 total LDH patients subjected to 1.25 U/mL condoliase and showed that 85.4% of patients had improved pain outcomes after six months or longer without severe adverse effects. A randomized controlled trial (RCT) by Matsuyama et al.25 of 194 LDH patients evaluated Condoliase at three doses of 1.25 U/mL, 2.5 U/mL, and 5.0 U/mL. They found significant pain reduction without significant differences in pain scores between doses. Notably, the occurrence of adverse reactions increased in a dose dependent manner, suggesting a single 1.25 U/mL dose may optimize outcomes. One study by Banno et al.26 evaluated clinical outcomes in 77 LDH patients that underwent condoliase therapy. At two years 76.1% of patients reported a ≥ 50% improvement to visual analogue scale (VAS) scores and did not require surgery while 11.9% proceeded with surgery due to ineffectiveness. No incidents of recurrent disc herniations were noted.
There exist studies suggesting that preexisting conditions and prior surgeries may represent contraindications for condoliase treatment. Banno et al.23 showed 47 LDH patients exposed to a single 1.25 U/mL condoliase dose at three months had significantly improved leg and back pain on VAS and Oswestry disability index (ODI). However, effectiveness was decreased in patients with a history of discectomies, spondylolisthesis, or a posterior intervertebral angle >5°.23 A retrospective single-center analysis by Takeuchi et al.27compared 101 patients with favorable and poor outcomes following condoliase. They found that calcification or ossification in disc hernia on CT scans and rates of a posterior intervertebral angle >5° were significantly more common in patients with poor outcomes. It is noteworthy that the study was limited by its small sample size with only 32 patients that underwent CT scans compared between the two groups. Overall, studies support the short-term effectiveness of condoliase as a safe and minimally invasive therapeutic approach. Nonetheless its long-term side effects as well as the length, timing, and indications to optimize patient outcomes remain unclear.
Cytokine antagonist, methylene blue, and mesenchymal stem cells are other intradiscal injection therapies that may reduce disc degeneration and promote repair. While there are experimental studies supporting the use of cytokine antagonists, anti-TNF etanercept and anti-IL6 tocilizumab, the lack of large-scale studies limit understanding of their usage in clinical situations.28,29 Injection of methylene blue has also been suggested to provide pain relief by dampening neural conduction in the nucleus pulposes.7,30,31 However, its efficacy remains unconfirmed due to a lack of recent clinical trials and limited understanding of its long-term effects. Mesenchymal stem cells are a promising approach for intervertebral disc degeneration (IDD) due to their ability to differentiate into nucleus pulposus cells, promoting the synthesis of the extracellular matrix, and secretion of anti-inflammatory factors.9 They have been demonstrated to provide pain relief and improve disc degeneration in patients with IDD and LBP.32,33 However, more studies are needed to confirm the efficacy and clinical indications for MSC with varying presentations, histories, and conditions such as low pH, high inflammation, and low oxygen.34
Laminectomy: Traditional Open Approach and Microdiscectomy
Laminectomies are the conventional treatment when no spinal instability is present and involves resection of the lamina to increase the neural foramen. Discectomies aim to cut the protruding intervertebral discs.11 Although they are often done simultaneously there is evidence suggesting that microdiscectomies provide similar benefits to open laminectomies. A prospective randomized study of 112 LDH patients11 showed open laminectomies are equally effective in reducing radicular pain compared to microendoscopic discectomies.11 Another prospective study of 885 patients comparing micro decompression to laminectomies35 demonstrated no significant differences in complications and effectiveness after one year. Thus, microdiscectomies seem to be equally effective in reducing radicular pain, but with significant benefits in surgical times, incision size, hospital stay duration, and blood loss.11,35
Endoscopic versus Microscopic Discectomy
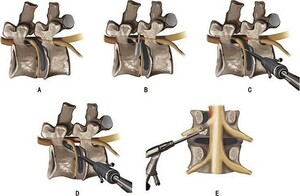
Both endoscopic and microscopic approaches to discectomy are minimally invasive with microscopic discectomy being the gold standard surgical treatment for LDH. However, recent evidence has demonstrated that percutaneous endoscopic lumbar discectomies (PELD) may be an effective alternative to microdiscectomies (Figure 1). A retrospective study by Kim et al*.*36 of 104 LDH patients demonstrated PELD had a high success rate of 96% in varying kinds of LDH including severely difficult and extremely difficult cases. Additionally, Liu et al.37 retrospectively compared the effectiveness of percutaneous transforaminal endoscopic discectomies (PTED) to microscope assisted tubular discectomies (MTD). They showed PTED was associated with shorter hospital stays, shorter incisions, less intraoperative blood loss, and lower rates of back pain in follow-ups 10-15 months post procedure. PTED was also suggested to treat foraminal and extraforaminal disc herniations more favorably as opposed to microscopic discectomies, especially in the posterior approach.37 In posterior approaches for far lateral LDH, PTED may damage the articular process joint and posterior structures of the spine less while microdiscectomies often have limited visual fields caused by less facetectomy. Collectively, the current evidence suggests benefits of using an endoscopic approach exist based on pain and post-operative criteria. However, more studies are needed to compare the utility of the various types of endoscopic approaches.
Tubular Discectomy, a Minimally Invasive Approach
The usage of a table-mounted set of tubular retractors with visualization via an endoscope or microscope has been proposed to potentially optimize clinical outcomes.13 However, recent studies have shown there may be no significant advantages in short- or long- term clinical outcomes using the tubular approach. A RCT by Overdecest et al. 38 involving 159 LDH patients for 260 weeks tested for sciatica lower leg and back pain, self-perceived recovery, and reoperation time at 2, 4, 6, 8, 12, 26, 38, 52, 78, 104, 156, 208, and 260 week intervals. Results found no significant differences in clinical outcomes between minimally invasive tubular discectomy and conventional discectomy at any point measured. Similarly, a review of 10 prospective trials showed tubular discectomies had equivalently good clinical outcomes with lower blood loss and shorter hospital times when compared to standard discectomies.13 While more comprehensive prospective studies are required to verify these findings, this medium-grade evidence suggests that the hypothesized benefits of minimally invasive tubular discectomies over conventional discectomies are not evidence-based. Future studies should elucidate the personalized benefits of using one approach over the other.
Percutaneous Laser Disc Decompression: A Non-Invasive Alternative
First proposed in 1984, percutaneous laser disc decompression (PLDD) is a financially appealing and minimally invasive alternative for LDH that uses laser energy to vaporize content within the nucleus pulposus and reduce intradiscal pressure (Figure 2).39 The reduction of intradiscal pressure causes the herniated nucleus pulposus to recede towards the center of the disc, relieving nerve root compression and causing symptom relief. A RCT by Van et al.40 showed significantly lower short-term healthcare costs for PLDD compared to conventional microdiscectomies as no hospitalization or anesthesia is required. This was coupled with an insignificantly different one-year quality adjusted life years between the two approaches suggesting PLDD with surgery when needed may be a cost-effective strategy for LDH patients.
The comparative effectiveness of PLDD versus conventional surgeries in reducing short term (less than one year) pain is well-supported according to patient questionnaires. A study by Kim et al.41 showed significant pain relief as per ODI and VAS from both epiduroscopic laser decompression and open lumbar discectomies in LDH patients, without significant differences in pain-related outcomes between the two groups after six months. Similarly, a randomized prospective trial by Brouwer et al.42 showed noninferiority between PLDD and conventional surgeries for LDH at 8 and 52 weeks based on the Roland-Morris Disability Questionnaire, suggesting a one-year strategy of PLDD followed by surgery if needed to be an effective treatment plan.42 However, conventional discectomies have been found to have significantly reduced risk of long-term complications such as reoperation. Klessinger43 showed that PLDD patients had a high reoperation rate of 26% receiving open surgeries with 78.9% of those reoperations being within the first year after PLDD. Altogether, the current evidence suggests PLDD is minimally invasive, safe, cost-effective, and effective as a one-year treatment plan that can be followed up with open surgery if needed. Nonetheless, long-term complications such as reoperation are greater in PLDD, and there are few comprehensive large-scale studies supporting the effectiveness of PLDD.
Transforaminal Foraminotomy to further alleviate Interforaminal pressure in difficult cases
Although percutaneous endoscopic lumbar discectomies are a popular approach for symptomatic LDH, very highly up migrated lumbar disc herniations (VHUM-LDH) are difficult to treat via traditional approaches; this is due to anatomical barriers that often hide the sequestered nucleus pulposus from being viewed endoscopically.44 Therefore, newer studies have proposed the use of a novel transforaminal endoscopic lumbar foraminotomy (TELF)(Figure 3). A study by Yu et al.44 assessed the efficacy of TELF on 11 patients with VHUM-LDH and found significant improvements to mean VAS, ODI, and JOA scores. Additionally, the MacNab criteria for pain relief demonstrated 10 patients as “excellent” with one patient being “good”. There are various endoscopic approaches for lumbar decompressions surgery including transforaminal, extraforaminal, laminar, and central based on the location, severity, and level of the disc herniation. A retrospective analysis of the various endoscopic approaches for lumbar decompression45 demonstrated that all types of surgeries significantly improved pain relief outcomes according to the ODI, VAS, and MacNab criteria. However, future studies are needed to compare the efficacies of the various endoscopic approaches for different locations of the lumbar stenosis.
Pre and perioperative Antibiotic Prophylaxis
It is well established that perioperative antibiotics decrease rates of wound infections during surgery. Yet, the most efficient parameters such as dosage, and timing of empiric antibiotic administration remain under debate. Since the early 2000s, a common consensus involved a single preoperative antibiotic.46 A retrospective study by Dobzyniak et al.46 demonstrated that there was no significant difference in infection risk between lumbar disc surgery groups that received one preoperative and at least 3 post operative doses (3 infected/201) versus a single preoperative dose (5 infected/435) suggesting that a single preoperative antibiotic dose was sufficient to minimize infection risk. Therefore, multiple antibiotic doses pre, peri, and post-surgery did not seem to provide any additional benefits and many hospitals employed a single preoperative antibiotic dose for lumbar disc surgeries. However, there are also studies suggesting multiple perioperative doses may maximize benefits. A study of all patients that underwent surgery at a large regional hospital between 2003-2014 compared the efficacy of a single dose (1g if patient <80kg, 2g if patient >80kg) cefazolin versus multiple prolonged doses (72h) of cefazolin intraoperatively, with ciprofloxacin as the replacement antibiotic.47 Results demonstrated that the surgical site infection rate was significantly higher for single dose (5.3%) versus multiple doses (2.2%) with data analysis showing that the multiple dose group was the most important differentiating factor. Even so, a plethora of evidence support insignificant differences between single versus multiple doses and the current North American Spine Society’s (NASS) evidence-based guidelines recommend the use of a single preoperative dose for uncomplicated laminotomies or discectomies.48
Various antibiotics such as vancomycin and cefazolin are employed preoperatively. A study by Lopez et al.49 demonstrated the introduction of a vancomycin and cefazolin protocol to be effective in lowering the post-surgical revision rate for surgical site infection. Furthermore, a prospective RCT50 demonstrated intra-operative intradiscal vancomycin powder to significantly reduce (1.4% infection rate) the rate of post-discectomy discitis compared to control (5.56% infection rate). It remains unclear which timing, dosages, and antibiotics are most effective for the specific comorbidities and clinical conditions of each patient.
Lumbar Disc Herniation Recurrence Post-Surgery
Recurrence following a microdiscectomy is a major post-surgery concern and has been found to occur in a range of 5-15% of LDH patients.51 Risk factors for recurrence include but are not limited to smoking, occupational lifting, preexisting diabetes, degree of joint degeneration, and factors associated with the primary discectomy.52 Miwa et al.53 has shown smokers have a high 18.5% recurrence rate as well as a high odds ratio of 3.472 versus nonsmokers. Preexisting diabetes mellitus is a significant risk factor, with a very high rate of recurrence of 28% versus 3% in control patients.54 Kim et al.55 evaluated 71 patients that underwent one-level discectomies and six-month follow up. Results showed that a reduction of disc height greater than 20% at follow-up was associated with a significantly greater recurrence rate (36.4% versus 14.3%). Additionally, grades 3 and 4 compared to grades 1 and 2 preoperative facet joint degeneration were statistically significant risk factors for recurrence (41.2% and 14.8% respectively). It is noteworthy that BMI has been considered an estimated risk factor for recurrence, but this correlation is poorly supported across various literature. For example, meta-analysis by Huang et al.52 which pooled 17 studies demonstrated no significant correlation between BMI or obesity with recurrent LDH.
Preoperative biomechanical parameters such as the patient’s disc height index (DHI) and sagittal range of motion (sROM) have been noted to have significant correlation with recurrent LDH. For instance, Kim et al*.*56 followed 159 LDH patients for 70 months and found significant correlation in both DHI and sROM; recurrence groups had a mean DHI and sROM of 0.37 and 11.3 respectively compared to a mean DHI of 0.29 and a mean sROM of 5.9 in the non-recurrent group. DHI has been correlated with disc degeneration due to annular collagen degradation which the authors accredit may cause the higher recurrence rate. Overall, these results suggest preoperative biomechanical parameters may be significant predictors for recurrent LDH.
The primary discectomy has also been shown to be an important factor influencing the rate of recurrence. A systematic evidence-based review by Watter and McGirt57 evaluated the effectiveness of aggressive and conservative discectomies along with the rate of recurrent low back pain and herniation. The benefits of conservative discectomies were demonstrated to be shorter operation times, quicker recovery time, and lower rates of recurrent lower back pain. However, conservative discectomies were shown to have higher rates of LDH recurrence (8.7%) than aggressive discectomies (3.3%). Although aggressive discectomies may decrease the risk of herniation, it also comes with accelerated loss of disc height which may predispose patients to degenerative disc disease. Therefore, the pros and cons of each discectomy should be carefully weighed and considered for each individual patient-surgeon encounter.
Annular Closure Devices to Reduce Recurrence
Recurrence is most prominent six weeks post-surgery, but can occur decades after intervention. Thus, prosthetic devices such as Barricaid™ and Annulex-Xclose have been proposed, of which Barricaid™ is the only currently FDA approved annular closure device (ACD). ACDs are synthetic mimics of the annulus, helping to contain the nucleus pulpous while decreasing the risk of reherniation.58 The Barricaid™ ACD is comprised of a titanium anchor portion fused into the vertebral body and a polyester fabric mesh that rests on the edge of the cartilage in the spine (Figure 4).14 This attempts to close the defect hole in the patient’s vertebrae and prevent reherniation. Many studies have supported the capacity of ACDs to prevent reherniations. A meta-analysis of 811 discectomy cases14 evaluated short-term (up to two years) effects of ACDs. Results demonstrated significant reduction (24 recurrence/811 cases) of recurrent herniations versus the control (51 recurrence/645 cases) with an odds ratio of 0.34 in control versus ACD Barrciaid or Annulex-Xclose. Furthermore, a systematic review with meta-analysis by Arts et al.59 compared 3947 LDH patients across 14 studies. They contrasted lumbar discectomies to discectomies and ACDs to conservative care. There was significant reduction of reherniation and reoperation in the discectomy and ACD group compared to discectomy alone, along with significantly greater reduction of leg and back pain in discectomy and ACD compared to conservative care. Thomé et al.58 had similar findings in a multicenter RCT of a 5-year follow up of 267 patients treated with microdiscectomies and ACDs versus 283 patients treated with just microdiscectomies. There were insignificant differences in pain scores and health related quality of life improvements between microdiscectomies and ACDs compared to microdiscectomies alone. However, the risk of associated symptomatic reherniation, reoperation, and serious adverse events were significantly lower in microdiscectomies with ACDs. Altogether evidence suggests the use of ACDs with discectomies may minimize recurrence without compromising the clinical benefits of surgery for up to 5 years post-operation. However, extensive decade long studies are needed to verify the long-term effectiveness of ACDs.
A recognized limitation of ACDs is that it can only be used in holes that fit between 4-6mm height and 6-12mm width; the implantation of Barricaid ACD is required to be in two locations, the intervertebral disc defect and the cartilage.60,61 Therefore, insufficient disc material prevents the implantation into the disc defect which represent a major limitation of the device. Although ACDs represent a major advancement in the treatment of LDH and its recurrence, future studies may improve ACDs to be more encompassing of the widely varied presentations of lumbar disc herniations.
Billing and Reimbursement
There are numerous studies evaluating the cost effectiveness of conservative care and surgical treatment modalities such as microscopic and endoscopic discectomies. Glennie et al.62 described an RCT comparing nonsurgical and surgical treatment for chronic radiculopathy; inclusion criteria consisted of posterolateral disc herniation at L4-L5 or L5-S1 with MRI-confirmed unilateral radiculopathy. Patients were randomized into early surgery or nonsurgical care with surgery if needed. Ultimately, 64 patients were included into each group with similar baseline characteristics. Patients were followed for up to two years, but all costs were incurred within one year. The study found costs were greater for operative modalities (CAD$4,161) than nonoperative modalities (CAD$3,113) and the quality-adjusted life-year (QALY) increase was significantly greater in the surgical approach as soon as three months status-post intervention. Both groups had a baseline QALY of 0.49 however, following year two, the surgical group reported a QALY of 0.76 ± 0.03 while the nonsurgical group reported 0.69 ± 0.03. This significant difference in improvement brings into question the potential for long term offset of surgical cost by superior economic performance in patients post-surgery.
Choi, Shim, et al.63 evaluated the cost of microdiscectomy and three different endoscopic techniques TELD, IELD, and UBED. Patients were included if they presented with sciatica and back pain refractory to conservative measures for at least six weeks and were followed for at least one year. Ultimately, 726 patients were included in the study, with 157 undergoing TELD, 132 IELD, 140 UBED, and 136 microdiscectomy. These procedures consisted of surgery from the L1-L2 to the L5-S1 levels. Underlying characteristics were similar among all patients. The authors found that microdiscectomy ($5,061.9) was significantly more costly than the endoscopic techniques ($4,413.6), and the QALY gain from endoscopic discectomy was significantly higher than for microdiscectomy. In this regard, endoscopic techniques are more cost effective at approximately $26,776.9 per QALY versus microdiscectomy at $34,840.4 per QALY.
The type of insurance that the hospital bills and the location of the surgery, free-standing ambulatory surgical centers (ASCs) or hospital outpatient facilities/departments (HOPD), should also be considered. Malik et al.64 performed a retrospective cohort study using data from the Humana Administrative Claims (HAC) database, which contains records from over 20 million enrollees in both commercially insured and Medicare Advantage enrollees. The authors queried the HAC from 2007 to 2014 for Current Procedural Terminology (CPT) codes 63030, 63056, and 0275T, which represent laminotomy with nerve root decompression, transpedicular approach with spinal cord decompression, and percutaneous laminotomy/laminectomy, respectively (further details may be found in the CPT code book). Exclusion criteria included two-level surgery, open laminectomies, fusions, revision discectomies, and/or deformities. The location of the surgeries was determined using service location codes 22 and 24, for HOPD and ASC, respectively. Ultimately, 11,552 patients met the criteria with 1,077 surgeries performed in an ASC and 10,475 were performed at an HOPD. After matching baseline characteristics, 990 patients were included in each ASC and HOPD group. The study’s ASC surgeries had an average of $5,814 and HOPD surgeries an average of $7,829 on Medicare Advantage plans. Commercial insurance plans were even more expensive, with ASC surgeries averaging $10,116 and HOPD surgeries averaging $13,623. In both insurance type subgroups, ASC surgeries were statistically significantly less costly than those at HOPDs. Of note, there was no significant difference in the rates of 90-day all-cause complications between ASC and HOPD surgeries, including wound, pulmonary, cardiac, thromboembolic, septic, urinary, and renal complications. This analysis naturally lends itself to support increased outpatient surgeries, when patient history and procedural complexity permits, in ASCs due to decreased costs. The authors hypothesize that this is partly due to the physician-ownership model of many ASCs, which incentivizes lower unnecessary resource utilization and cost.
Reimbursement rates based on Medicare national averages should also be utilized in surgical decision making. DePuy Synthes compiled a CPT code book with associated average Medicare costs for individual CPT codes.65 Spinal decompression Medicare reimbursement rates range from $1,005 to $1,838; the exact costs differ depending on the type of laminectomy/laminotomy, the level of spine operated upon, and the approach type. Spinal instrumentation also incurs costs and may range up to $823 for primary instrumentation. Finally, outpatient services are noted to have significant differences between HOPD and ASC groups. In line with the findings of Malik et al.,51 HOPD services generally average at $6,265 while ASC services average at $2 944. The notable exception is percutaneous laminotomy, which costs less for both HOPD and ASC settings.64,65
Taken together, the above studies and CPT code books should be considered when recommending different treatment modalities to patients. Cost considerations carry significant weight in decision making but other components, such as a potential increase in QALYs, should be contemplated. This is particularly true for those patients who are active and working-class members of society, as time unable to work may be costly to the patient, their families, and society. These “hidden” costs of spinal pathologies may outweigh the calculated costs of surgery and thus should be utilized during the patient-physician decision making process.
Conclusion
Lumbar disc herniation remains one of the most common causes for LBP worldwide. The treatments for LDH have improved in both scope and quality, from interventional pain therapies to various surgical approaches to post-surgical management of recurrence. Non-surgical pain intervention is often the initial approach for symptomatic LDH. Interventions include intradiscal injections of 1.25U/mL of condoliase, methylene blue, and mesenchymal stem cells, all of which have preliminary results supporting their use as safe and effective treatment approaches for LDH. However, the lack of long-term and comprehensive studies on these approaches limits the extent to which we can apply them in clinical practice. Microdiscectomies remain the gold standard surgical approach, and alternative approaches such as tubular discectomies, PLDD, and transforaminal foraminotomy may yield similar symptomatic relief with better clinical outcomes such as lower blood loss and shorter hospital stays. To prevent infections during surgery, pre and perioperative antibiotic prophylaxis have both shown effectiveness with emphasis on a single preoperative dose being the standard for many lumbar spinal procedures. Post-surgery recurrence of LDH remains a major concern which is exacerbated by risk factors such as smoking, occupational lifting, degree of joint degeneration, sagittal range of motion, and conservative discectomies. However, recent advances in ACDs have shown that their implantation alongside microdiscectomies represent a promising intervention to reduce the rates of recurrence. Lastly, the cost-effectiveness of various procedures related to insurance, Medicaid, and CPT codes was discussed. Overall, the breadth and scope of treatments for LDH have vastly evolved over time, and understanding their implications may ultimately serve as groundwork for future approaches to optimize patient outcomes.
Some limitations of this study are that the literature reviewed in this study was limited to PubMed and Google Scholar and only articles available in English were considered. Additionally, there were varying methods of measuring outcomes and different patient populations. This limited direct comparison between articles and future studies are needed to access the optimal conditions for different treatment modalities.
Acknowledgements
Shaya Shasavarani MD – for providing advice and support to move the paper forward.
Austen Katz MD – for providing advice and support to move the paper forward.
Contributions
Bongseok Jung: Conception, writing, literature review, editing
Justin Han: Writing, editing
Junho Song: Literature review, editing
Alex Ngan: Literature review, editing
David Essig: Supervision, review, editing
Rohit Verma: Supervision, review, editing
Conflict of interests
The authors declare no potential conflict of interests.
Funding
None.
Availability of data and materials
All data and materials are available within the text.
Informed Consent
Not required.


_herniated_disc__b)_pldd_treating_the_herniation__c)_after_pldd_treatment__d)_ct_after_p.jpeg)


_herniated_disc__b)_pldd_treating_the_herniation__c)_after_pldd_treatment__d)_ct_after_p.jpeg)

