Introduction
The dislocated humeral head fracture associated with ipsilateral humeral shaft fracture is a rare injury. Some articles regarding two-part or three-part humeral head fracture-dislocation combined with humeral shaft fracture are reported, however, these articles are limited to case report or case series.1–5 The condition usually occurs in the elder population over 60-year-old with high-energy mechanical trauma or in osteoporosis population with low-energy mechanism. Different treatment protocols are applied among authors; thus, the optimal one is still a controversial issue. We report a successful clinical case by MIPO protocol with the essential purpose of providing a different perspective of treatment.
Case Presentation
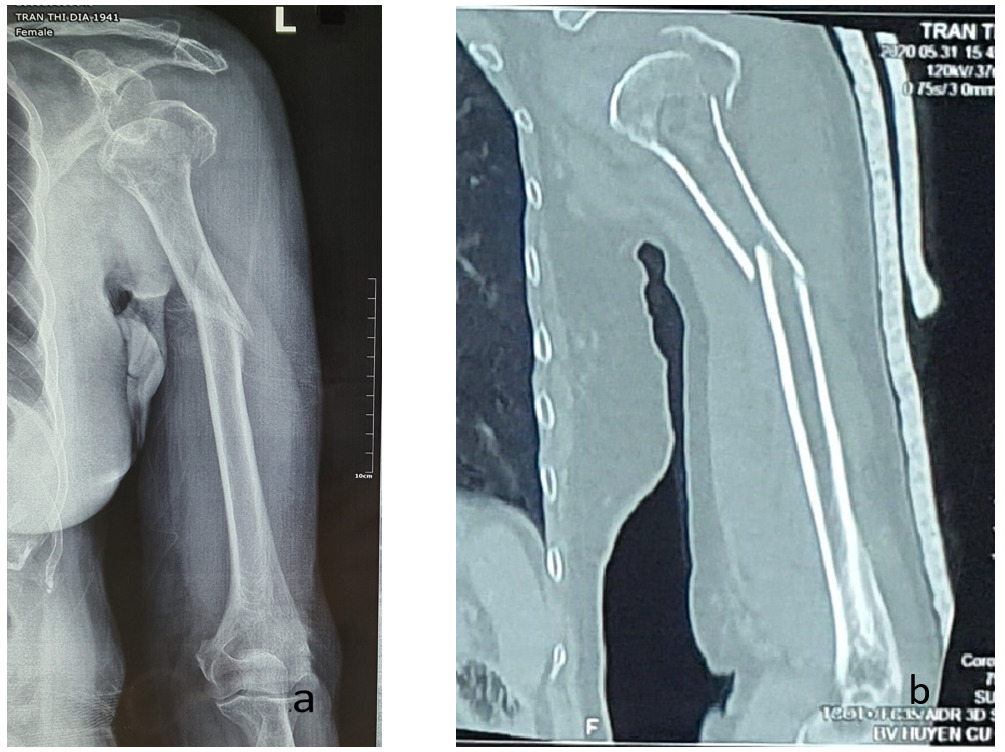
A 79-year-old female was referred to our emergency department with a painful left arm shortly after slipping on a wet floor. Initial assessment revealed no life-threatening injuries, severe pain and swelling from her shoulder to the middle third humerus, angular deformity in the middle third, bony crepitus palpable in the injured site, and no neurovascular impairment. X-ray delineated that a three-part humeral head fracture involved greater tuberosity and surgical neck fragments, anterior glenohumeral dislocation, and spiral fracture of the humeral shaft. A shoulder CT scan was indicated to obtain further information for operative planning, demonstrating a three-part fracture with little bone loss; and a calcar fragment > 8mm and its displacement < 2mm (Fig 1).
Ethical Considerations
We present a case report that doesn’t require ethical review or approval. We ensure that the patient has already been informed and consented to the protocol management and publication in Orthopedic Reviews Journal.
Management and Outcomes
The patient was operated in beach-chair position with a small pillow under the ipsilateral scapula to isolate the injured arm. Under general anesthesia, a 6-cm incision was made corresponding to the traditional deltopectoral approach. Blunt dissection then was performed to expose the fracture without soft tissue impairment. The dislocation-fracture of the humeral head was delicately reduced and temporarily fixed by 1.8-2.0mm Kirschner wires under fluoroscopic imaging. A technical tip was the usage of Kirschner wires as joysticks associated with Fiber suturing through infraspinatus tendon footprints to manipulate the great tuberosity fragments. A 7-hole PHILOS (Synthes) plate was percutaneously placed across the humeral shaft fracture for definitive fixation of the combined fractures (Fig 2). The plate was bent in a helical fashion in the middle third of the plate. A 3-cm incision was made in the distal fragment to control the distal position of plating, followed by another 1.5-cm incision in the middle to add a cortical screw compressing the plate on the bone, finally adding locking screws under fluoroscopic imaging to accomplish osteosynthesis. Because of the large greater tuberosity, which was not completely stabilized by the PHILOS plate, a 2.0mm K-wire was not withdrawn to increase its stability. A degenerative supraspinatus tendon tear was found when exposing the humeral head, and repaired to its footprint by a transosseous suture procedure. Incised wounds were carefully closed without drainage.
Postoperatively, a rotator cuff brace was indicated for six weeks to protect the rotator cuff repair. The patient was transferred to a physiotherapist for enhanced recovery after surgery (ERAS) protocol. Scapulothoracic mobilization was encouraged immediately at the first postoperative days. PROM of shoulder was steadily increased from the 2nd to 6th week. Associated AROM was allowed from the 4th week and gradually converted to full AROM in the 12th week. Moreover, bisphosphonate and daily calcium - vitamin D3 were prescribed for management of osteoporosis and prevention of refracture. The formation of the soft callus occurs in humeral head fracture and humeral shaft fracture, respectively in the 8th week and 12th week. The patient complained about the irritated protrusion of K-wires in the proximal fracture site, which was removed in the 12th week then. After thirty-three months, the fractures were completely healing without avascular osteonecrosis of the humeral head and good shoulder function with 73 points Constant-Murley (Fig 3).
Discussion
Humeral head fracture associated with ipsilateral humeral shaft fracture was seen as a rare condition. We searched on many published resources and found not many articles regarding this issue, especially series case. We found three articles reporting three-part fracture dislocation of the humeral head associated with ipsilateral humeral shaft fracture with different operative protocols.
Flint et al. (2008) described a 69-year-old female who sustained a three-part humeral fracture with anterior dislocation, three-part humeral head fracture and concomitant humerus shaft fracture was conservatively treated due to operative rejection.3 The patient ended with a good outcome, however, the author recommended conservated treatment is not suitable for those young and high-level functional demand.
Tomás Pérez Cervera et al. (2016) reported a 63-year-old male who sustained a three-part humeral fracture-dislocation involved with anatomical neck and great tuberosity, ipsilateral humeral shaft fracture.5 The patient got an iatrogenic injury of the axillary artery when the first attempt at close reduction of the fracture-dislocation. The combined fractures were treated 5 days ago with cemented stem hemiarthroplasty associated with a long proximal humeral plate. The outcome was good eventually.
Guillaume Herzberg et al. (2017) reported an 84-year-old male who suffered similar injuries was operated with a long stem shoulder hemiarthroplasty associated with screw osteosynthesis of humeral shaft fracture.4 The patient had a good to excellent result after thirty months of follow-up.
The above articles showed that conservative treatment could be a good indication for old patients or those having low-level functional demands but for those young and high demands. Arthroplasty associated with osteosynthesis could be a good alternative protocol, however, intervention has much complexity, invasion, and a high risk of operative complications, especially in old patients with comorbidities. In our case, we performed MIPO protocol for the combined fracture with well-defined bone healing, good shoulder function, and cosmetics. Bone graft was no need due to little bone loss in CT scan.
The vascular supply of the proximal humerus originated from the anterior circumflex humeral artery and posterior circumflex humeral artery. Hertel et al. measured humeral blood supply by Doppler laser and discovered that if the calcar fragment of humeral head fracture is measured over 8mm and displaced below 2mm, the risk of avascular necrosis of humeral head is significantly low due to no impairment of its blood supply.6 In our case, the imaging findings (CT scan and X-ray) showed the calcar fragment with measurement above 8mm and minimal displacement, thereby reflecting a low risk of avascular necrosis. As a result, osteosynthesis is considered as a reasonable option for this case.
In studies conducted by Ugur G onç,7 Riccardo Luigi Alberio,8 and Dario Attala,9 MIPO with delta splitting approach is reported as a safe and effective option for three-part proximal humeral fractures. Manipulation of multifragmentary proximal humeral fractures through a small lateral anterior window is technically high demand, meanwhile, W Kongcharoensombat et al. demonstrated that a 5-cm safe zone from the lateral edge of acromion described in traditional literature is not suitable for Asian regarding thread to the axillary nerve.10 Recent studies showed MIPO through the deltopectoral approach had safety and good results when treating proximal humeral fractures as well as humeral shaft fractures.11,12 Furthermore, when reduction failed with MIPO through the deltopectoral approach, it’s quite easy to convert MIPO approach into the traditional deltopectoral approach as a backup plan. Consequently, we preferred MIPO through deltopectoral for treating our case.
Conclusion
Three-part humeral fracture-dislocation associated with ipsilateral humeral shaft fracture is rare with few cases reported by different protocols. We present a case successfully treated by MIPO protocol. MIPO shoulder be considered as a safe and effective option, however the risk of traumatic osteonecrosis of the humeral head is taken into account before operation decision-making.
Acknowledgements
We wish to thank all authors for their contributions, associations and cooperations in this article.
Author Contribution
Nhat Pham Van: Conceptualising the plan for surgery, performing the surgery, follow up patient’s recovery, writing the literature review for case report, reviewing the manuscript.
Hieu Nguyen Chi: Completing the manuscript, submission of the article, writing the literature review.
Tuan Nguyen Anh: Assisting the surgery, analyzing the radiology and MRI.
Xuan Tran Chanh: Assisting in planning and in the surgery, writing the draft for case report.
Tuan Nguyen Anh: Assisting in planning and in the surgery, writing the literature review, taking note of postoperative functions.
Conflict of interests
We declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Minimal invasive plate osteosynthesis for the dislocated humeral head fracture associated with ipsilateral humeral shaft fracture: A case report.


_3_mini_incisions_were_made_in_mipo_approach._(b)_(c)_fluoroscopic_images_checked_the_b.png)
_x-ray_in_33_months_of_follow-up_showed_good_fracture_healing_without_osteonecrosis_of_.png)
_3_mini_incisions_were_made_in_mipo_approach._(b)_(c)_fluoroscopic_images_checked_the_b.png)
_x-ray_in_33_months_of_follow-up_showed_good_fracture_healing_without_osteonecrosis_of_.png)