1. Introduction
Vertebral osteomyelitis (VO), also known as spondylodiscitis, refers to a spectrum of spinal infections ranging from isolated vertebral osteomyelitis and/or discitis to diffuse infection with associated epidural abscess.1 It can present in a number of ways, from an isolated lesion in a neurologically intact patient to a critically ill patient in septic shock with spinal instability and/or neurological compromise.2,3
Treatment is often guided by the status of the patient at the time of clinical presentation. Patients with a known organism who are clinically stable without evidence of spinal instability can often be treated with an initial course of antimicrobial therapy. Surgery is often required in patients with sepsis, spinal instability, neurological compromise, (such as weakness, paralysis, or bowel/bladder dysfunction), or in chronic cases where medical treatment has previously failed.4,5
The appropriate surgical treatment varies based on the nature of the infection and the condition of the patient. Lesions that are otherwise stable may sometimes require procedural biopsy of the inflammatory tissue in question to help guide antibiotic therapy. Patients without instability who have failed medical treatment and require debridement or decompression of the neural elements may be treated with isolated decompression and/or debridement alone.6 If the infection has progressed to the point at which it disrupts the mechanical stability of the spine, or if obtaining adequate decompression warrants a degree of bony resection that destabilizes the spine, spinal fusion may be required.7,8
While the role of systemic antibiotic therapy is well established in the treatment of VO, there is not a standardized method of local antibiotic delivery. A variety of techniques are utilized in orthopaedic surgery for local antibiotic delivery, including application of local antibiotic powder to the wound, use of antibiotic beads, and the use of antibiotic bone cement.9
Although antibiotic bone cement (ABC) is commonly utilized in other orthopedic subspecialties such as adult reconstruction/joint arthroplasty, the routine use of ABC in spine surgery is not well established. The purpose of this manuscript is to review the principles and techniques associated with the use of ABC in orthopaedic surgery and to broaden its applications to spine surgery. This will be illustrated with several case examples.
2. Established Clinical Uses of Antibiotic Cement in Orthopaedic Surgery
Bone cement has been routinely used in orthopaedic surgery since 1870, when Themistocles Gluck, a German surgeon, pioneered its use for the fixation of a total knee prosthesis.10 Early bone cement consisted primarily of plaster and colophony. In 1960, Sir John Charnley introduced polymethyl methacrylate (PMMA), which has become the gold standard for cemented fixation in total joint arthroplasty.11 PMMA acts as a space-filler to ensure a close mechanical interlock between the bone and the prosthesis.10 Buchholz et al. further expanded the use of bone cement by demonstrating that it was capable of releasing substances like antibiotics and copper ions from its surface.12 Since this discovery, PMMA cement impregnated with antibiotics has been a key component in the treatment of prosthetic joint infections through local antibiotic delivery. Over the years, the use of ABC has expanded, and many surgeons utilize antibiotic cement for infection prophylaxis in both primary and revision joint replacements.
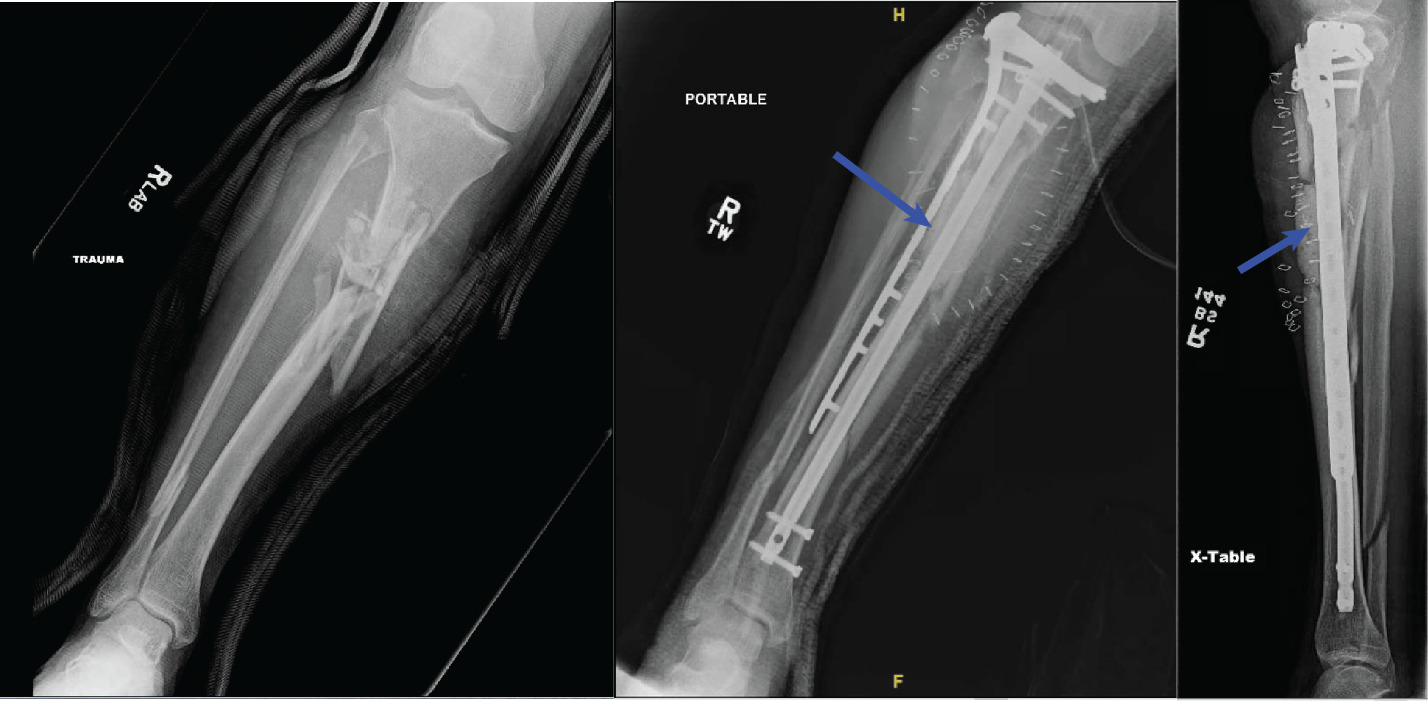
Bone cement can also address segmental bone defects in orthopedic trauma surgery. Masquelet et al. describe a technique that combines induced membrane formation technology with bone grafting for the management of long (> 5 cm) diaphyseal defects in poorly vascularized, infected, and/or irradiated sites (Figure 1). The induced membrane’s unique biological and structural properties act as an envelope that preserves and protects the bone graft and aids in the revascularization process. The Masquelet technique is a two-stage process which may also be applicable to spine surgery. The first stage involves extensive debridement of devitalized tissue with osseous stabilization across the bone graft. The osseous void is filled with a PMMA cement spacer, often loaded with antibiotics, which prevents soft tissue invasion of the defect. The second stage is performed after 6-8 weeks or when the tissue is healthy. At this point, the biomembrane around the spacer is incised and the spacer is removed and replaced with bone graft around the induced membrane to allow for osseous integration across the bone defect.13,14
Antibiotic cement has also been used in the form of antibiotic cement beads. After setting, antibiotic beads can be introduced to a surgical site where they provide local wound control through antibiotic elution. Recent studies have demonstrated this technique to be effective in treating spinal surgical site infections.15,16
3. Efficacy & Safety
Antibiotic-loaded cement spacers play a role in both the prevention and treatment of extremity infections. A systemic review revealed that prophylactic use of ABC in hip and knee replacements led to a 20 to 84% risk reduction of prosthetic joint infections (PJI).17 Leong et al. utilized the National Joint Registry for England to reveal that patients undergoing primary total hip arthroplasty with ABC had lower rates of revision for PJI.18 Wang et al. performed a meta-analysis and discovered that prophylactic utilization of ABC reduced deep infection rates but not superficial infection rates after primary arthroplasty.19
In a study of 27 patients with open fractures and long segmental defects, the Masquelet technique with antibiotic cement led to zero long term residual infections.20
Additionally, Masquelet retrospectively reviewed 18 of his patients that underwent his induced membrane technique with a follow-up of 10-22 years. There were no cases of recurrent infection in the reconstruction zone in any of the patients.21
Safety concerns have been raised regarding the use of ABC. These concerns include local toxicity, monomethyl methacrylate (MMA) vapor exposure, allergic response, structural compromise, inhibition of bone formation, and the development of drug-resistant bacteria.22–32 However, numerous studies confirm that ABC is safe and effective in the majority of patients.19,33–36
4. Cement Properties and Technique in Spine Surgery
Cement utilized in extremity surgery primarily consists of PMMA. PMMA is an acrylic polymer formed by mixing liquid MMA monomer and a powdered MMA-styrene co-polymer.37 The liquid monomer polymerizes around the powdered particles to form the hardened cement through an exothermic reaction.10 (Figure 2) PMMA often contains a radio-opacifier such as barium sulfate which allows for radiographic visualization of the cement.37
Several different commercial PMMA products are available that have distinct qualities. (Table 1)
During the polymerization process, surgeons can add antibiotic powder, which allows for local antibiotic delivery.38
Bone cement has been used widely in spine surgery to augment fixation in osteoporotic bone.39,40 Mechanically, bone cement increases pedicle screw fixation pullout strength.41 Previous studies have shown some decrease in structural integrity of bone cement when augmented with antibiotics.28–30 Although these structural concerns are valid, ABC is not primarily used in the spine for structural support–rather it is a vehicle for antibiotic delivery. In this light, the addition of cement, irrespective of antibiotic impregnation, would result in a net improvement in structural support. The relatively diminished integrity of antibiotic-treated cement compared to cement without antibiotics is more of a concern in cases in which cement is primarily used for structural stability, such as in a load-bearing joint like the hip or knee.
Choice of antibiotic is based on the identified or suspected organism. (Table 1)
5. Technique For Utilization
Different PMMA products and antibiotic concentrations can affect cure time and often require surgeon familiarity with the different cement products and antibiotics to accurately predict curing.
5.1. Curing
The curing of ABC is divided in to 4 phases: 1) mixing; 2) handling (sticky); 3) working (doughy); 4) hardening.
During the mixing period, which generally takes about one minute, the liquid monomer is mixed with the powder and antibiotics. This can be done either by hand or with the assistance of vacuum suction devices.38 The handling period is the time it takes for the compound to reach a consistency state where it is doughy enough to be delivered to the tissues for its intended state, known as the working state. The hardening period is the time it takes for the cement to fully harden after delivery, or until it can no longer be delivered.10
Bone cement is heat sensitive, and variations in room or tissue temperature or humidity can affect the characteristics and setting time of the cement.56,57 Lower temperatures can increase the handling, working, and hardening periods, while higher temperatures can conversely decrease these phases.58 Manual handling of the cement can also accelerate the curing process.38 Although exact requirements vary from product to product, in general, ABC should be utilized at a temperature of 73 degrees F (23 degrees C).59
5.2. Application of cement
Cement can be delivered to the spine in various ways depending on the intended usage. It can be delivered manually to the spine to fill large defects in the vertebral body or disc space.60,61 Some surgeons have also described coating the instrumentation constructs with cement to minimize the risk of local infection and biofilm formation.62,63
Multiple delivery methods exist to allow for direct delivery to the vertebral body. For instance, the following case examples describe treatment of VO by augmenting pedicle screws with ABC in the local environment. One method to do this is to inject cement directly into the vertebral body after cannulating the pedicle screw tracts, in a manner similar to vertebroplasty or kyphoplasty. This is immediately followed by placement of the pedicle screws into the cemented path before the cement fully hardens. Several manufacturers also make fenestrated pedicle screws that allow for direct delivery of cement to the vertebral body through the cannulated screw. (Figure 3) This can allow for efficient cement augmentation across multiple vertebral bodies. Surgeons should closely scrutinize imaging during this process to watch for cement extravasation.
5.3. Complications of Cement Delivery
Although antibiotic cement may be a powerful resource in the treatment of spine infections, usage of ABC may be associated with several complications and should be carefully planned and closely scrutinized. Surgeons should be mindful of the potential for cement extravasation, especially when the bone is weakened secondary to infection, tumor, or fracture. Cement can extravasate posteriorly into the canal, which can cause emergent neurological deficits (Figure 4), can extravasate anteriorly to the vertebral body and damage visceral structures, and in some cases has the propensity to enter the vasculature, which can lead to cement embolization (Figure 5).
Given the heat generated during the exothermic curing process, damage to neural structures can occur due to thermal injury.64,65 This is of particular concern in cases of extravasation where cement could come into direct contact with sensitive neurovascular structures
Of note, cement can make revision cases more difficult. Cemented screws that have failed can compromise bone stock and make it difficult to achieve revision transpedicular fixation, often warranting an extension of prior surgical constructs. Moreover, if an infected vertebral body is treated with ABC and then progresses to the point of requiring further surgery, the subsequent case could be substantially more challenging. An example of this is in the setting of a cemented vertebral body, which might require corpectomy.
5.4. Case Example
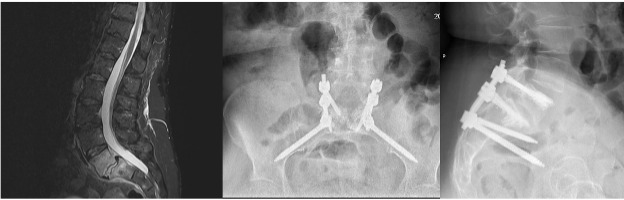
A 57-year-old female was initially admitted to an outside facility and found to have L5-S1 osteodiscitis with a ventral epidural phlegmon and blood cultures positive for Methicillin-Sensitive Staph Aureus. She was treated for 6 weeks with Oxacillin with persistent low back pain, as well as persistently elevated inflammatory markers. Repeat imaging revealed progression of her osteodiscitis at the lumbosacral junction with development of spondylolisthesis (Figure 6). Given her failure to respond to medical treatment, she was treated with surgical decompression, debridement of osteodiscitis, and stabilization from L5 to the pelvis with ABC augmentation of her pedicle screw fixation. Postoperatively, she remained on antibiotics for 6 weeks with gradual improvement in her back pain and normalization of her inflammatory markers.
6. Conclusion
Antibiotic-loaded bone cement has been widely used in orthopedic surgery for more than 150 years, both for prophylaxis and treatment of bacterial infection. Efficacious results have been observed in both settings.66 However, little literature exists regarding the use of ABC in the field of spine surgery. With a thorough understanding of the properties of the cement and the methods of delivery, ABC is a useful adjunct in the treatment of spinal infections.
Acknowledgments
We want to thank Stryker/K2M for providing and allowing the usage of the picture of the fenestrated screw.
Correspondence
Alan H. Daniels, MD
Department of Orthopedic Surgery
Warren Alpert Medical School, Brown University
Providence, RI 02906
Phone: 401-330-1420
Fax: 401-270-3378
Email: alandanielsmd@gmail.com
Author Contributions
Conceptualization, EO, CO, GA, AD; methodology, EO, CO, GA; software, CO, GA; validation, EO, JAY, AD; formal analysis, CM; investigation, CO, GA, CM; resources, CM, JAY; data curation, GA, CM; writing—original draft preparation, EO, CO, GA, CM writing—review and editing, EO, CO, GA, CM, JAY, AD; visualization, CO, CM, JAY; supervision, EO, AD; project administration, AD; funding acquisition, AD. All authors have read and agreed to the published version of the manuscript
Declaration of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Alan H. Daniels receives consulting fees from Stryker, Orthofix, Spineart, and EOS, research support from Southern Spine, and Fellowship support from Orthofix.
Eren O. Kuris receives consulting fees from Spineart and Seaspine
GA, CO, and CM report no disclosures.
Funding
This research received no external funding