Introduction
There are now over 1.3 million primary knee replacements recorded in the United Kingdom (UK) National Joint Registry (NJR), the world’s largest arthroplasty registry. Approximately 90% of these are total knee replacements (TKRs) with the remaining being partial knee replacements.1 The global number of primary knee replacements has been increasing tremendously annually and in the United States of America (USA) it is estimated that by 2030 demand for primary TKRs would grow to 3.48 million procedures per year.2 In keeping with this trend, the number of knee revisions has been on a steady incline with 1,225 revisions performed in the UK in 2004 and 7,005 in 2019.1 Although Theophilus Gluck is often credited with performing the first ever TKR in 1891, reports of periprosthetic fractures (PPFs) remained scarce and only began appearing in the late 1970s.3 It wasn’t until the last two decades that PPFs became more frequently spotlighted with published incidences ranging from 0.3% to 3.5% for distal femoral PPFs, though large joint registries estimate the rates to be between 1.1% and 1.3%.4–6 Of the 87,535 revision procedures recorded in the UK NJR, 3,358 revisions (3.84%) were performed for a PPF. Data from the Scottish arthroplasty project has demonstrated that the number of PPFs recorded per year has more than doubled between 1997 and March 2008 in line with the increase in TKRs performed.7 This rise in the number of procedures performed reflects the number of at-risk implants in the UK NJR dataset and the wider population.
There is significant mortality and morbidity associated with distal femoral PPFs and despite advances in our understanding of fracture management and implant design, the subsequent reduction in quality of life and joint function remains high. Mardian et al. reported only 20% of patients were able to mobilise without assistance postoperatively.8 This perhaps may account for the findings of two studies by Shields et al. and Streubel et al. which demonstrated mortality rates of 14% at 3 months and 17.7% at 12 months postoperatively, with 80% of the deaths occurring within 3 months of surgery.9,10 In the UK, the national hip fracture database has recently been collecting data on PPFs and it has been recommended that these fractures should be considered life-threatening injuries that need to be approached with the same urgency and treatment objectives as native hip fractures (e.g. early mobilisation and weightbearing) to improve the prognosis for patients.10–12
Unfortunately, these fractures remain challenging to treat owing to a number of factors including the advanced age of patients and the difficulty in achieving stable fixation in patients with poor bone stock and fragile bone quality. The primary aim of this article is to provide a meta-analysis of specific outcomes (infection, non-union, re-operation, and mortality) of locking compression plates (LCPs) and retrograde intramedullary nailing (RIMN) for distal femoral PPFs around TKRs.
Methods
Literature search strategy
This systematic review and meta-analysis was conducted in adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.13 Searches were conducted on PubMed/Medline looking at literature published between January 2012 and December 2022. The search terms were as follows: ‘Total knee arthroplasty (All Fields) OR Total knee replacement (MeSH Terms) AND Periprosthetic Fracture (All Fields) OR Peri-prosthetic Fracture (MeSH Terms)’. Articles generated were then screened and excluded in accordance with outlined eligibility criteria.
Eligibility
Inclusion criteria: articles published in the last 10 years (January 2012 to December 2022), patients aged 55 years and older, primary procedures (revision procedures of failed fracture treatment not included), minimum post-operative follow up of 6 months, articles of evidence levels I-III and English language texts only. Procedures included were RIMNs and LCPs.
Exclusion criteria: non-traumatic indications for arthroplasty, patients under 55, native bone fractures, case series, reports, letters, conference articles and abstracts, repeated studies and data, cadaveric and animal studies and studies deemed poorly designed and of evidence levels IV-V. Procedures excluded were revision arthroplasties, distal femoral replacement (DFR), combination fixation strategies (LCP + RIMN hybrids), external fixation and conventional non-locked plating.
Data extractions and analysis
The authors independently extracted data from the selected articles, with discussions held for any disputes in extracted data. Study author, publication year, patient demographics, details of the intervention and outcomes were collated onto a spreadsheet using Microsoft Excel 16.64.
Review Manager 5.3 was used for data analysis. Mean difference was used to analyse continuous data, and odds ratio and the risk difference was used to analyse discrete data. Statistical significance was defined as P < 0.05, with confidence intervals of 95%. Chi squared was used to assess for heterogeneity in the pooled studies, with results represented through I2. I2 cut offs for defining heterogeneity were as outlined in the Cochrane Handbook for Systematic Reviews of Interventions, 0-40% = Low, 30-60% = Moderate, 50-90% = Substantial 75%-100 = Considerable.14 Results, along with all studies featured in the meta-analysis, were presented as forest plots.
Outcome Measures
The primary outcome measures of this review were postoperative rates of non-union, re-operation, infection and mortality. Data reporting complications, time to union, malunion, post-operative range of motion, refracture and patient reported outcome measures (PROMS) were also collected.
Methodological Quality
With consideration of the non-randomised nature of the selected studies, the methodological index for non-randomized studies (MINORS) criteria was used to score their methodological quality.15 Global scores were taken of each study, with a maximum score of 24 for comparative studies, and 16 for the non-comparative studies.
Results
Literature Search
The literature search initially produced 969 articles. These 969 articles were screened by reviewing their title and abstract. Of the screened articles, a final 10 were included in this review for assessment. The PRISMA flow diagram is below (see Fig. 1). Exclusions were made in accordance with the listed eligibility criteria. Of the included studies, 9 were retrospective cohort studies and 1 was a prospective cohort study.
Quality Assessment
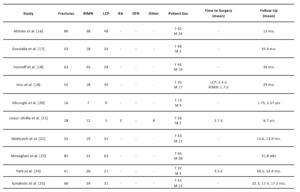
The methodological quality of the included studies was assessed using the methodological items for non-randomised studies (MINORS) criteria,15 all included studies were deemed to meet quality standards (see Table 1).16–25
Study Characteristics
Across all included studies a total of 536 PPFs were reported. 318 LCPs and 218 RIMNs were performed. The characteristics of all 10 included studies (see Table 2),16–25 and further outcome measures (see Table 3)16–25 have been outlined. An overall summary of our results is provided in Table 4.
Non-union
49 (9.4%) cases of non-union were reported in a total of 519 patients across 10 studies comparing RIMN and LCP, with moderate heterogeneity (I2 =44%). Comparative analysis found no statistical significance (P = 0.63) (see Fig. 2).16–25
Re-operation rates
67 (12.9%) cases of re-operation were reported in a total of 519 patients across 10 studies comparing RIMN and LCP, with moderate heterogeneity (I2=61%). Comparative analysis found no statistical significance (P = 0.86) (see Fig. 3).16–25
Infection
11 (2.4%) cases of infection were reported in a total of 460 patients across 7 studies comparing RIMN and LCP with low heterogeneity (I2=0%). Comparative analysis found no statistical significance (P = 0.80) (Fig. 4).16,18,19,22–25
Mortality
14 (5.5%) mortalities were reported in a total of 253 patients across 5 studies comparing RIMN and LCP, with low heterogeneity (I2 = 0%). Comparative analysis found no statistical significance (P = 0.68) (Fig. 5).16,17,19,20,22
Discussion
The aim of this meta-analysis is to provide an updated review of the literature for the treatment of distal femoral PPFs over the last decade, focusing on the rates of complications of RIMN and LCP. This study suggests that the rates of complications following RIMN and LCP performed for distal femoral PPF, are comparable. The overall incidence of complications reported were: non-union 9.4%, re-operation 12.9%, infection 2.4%, and mortality 5.5%. This meta-analysis found no statistically significant difference between RIMNs and LCPs in rates of non-union (9.2% vs 9.6%), re-operation (15.1% vs 11.3%), infection (2.1% vs 2.6%) and mortality (6.0% vs 5.2%) (respectively).
The results of this meta-analysis support the findings of recent meta-analyses by Magill et al. and Shin et al., both of which also reported no significant difference in rates of non-union and re-operation between the two surgical techniques.26,27 In addition, Shah et al. described no difference in rates of non-union, but did report a significantly lower re-operation rate following LCP compared to RIMN.28 Whilst this meta-analysis did find a lower rate of re-operation after LCP compared to RIMN, this comparison did not reach statistical significance. It is worth noting that two studies in this comparison did reach statistical significance for a lower re-operation rate post-LCP and that this comparative analysis showed moderate heterogeneity (I2 =61%), highlighting the need for further high-quality research into re-operation rates in particular before any substantial conclusions can be made.18,22
The aetiology of each complication was variably reported across studies. Only Hou et al. and Matlovich et al. reported on the aetiology of non-union following RIMN, with Hou et al. citing infection and distal screw loosening for their single case of non-union and Matlovich et al. citing one case of infection and one case of aseptic loosening.19,22 Hou et al. reported this case eventually requiring definitive management with above knee amputation but Matlovich et al. did not describe how the two cases of non-union were managed.19,22
Four studies reported on the aetiology of non-union following LCP.16,17,19,21 Aldrian et al. described three cases of plate breakage but did not disclose the aetiology of the other four cases of non-union following LCP. However, all seven of the cases reported by Aldrian et al. were managed by revision LCP and bone grafting.16 Lizaur-Utrilla et al. reported one case of non-union after LCP caused by loss of plate fixation which was managed with revision to a dynamic condylar screw. The other two cases of non-union described by Lizaur-Utrilla et al. were managed by dynamic condylar screw fixation for one patient and conservatively in the other, until a delayed knee arthrodesis was performed for loosening of the femoral component.21 Gondalia et al. reported all seven cases to be due to screw failure: five broken screws and two due to screw pull out.17 Hou et al. reported two cases of plate breakage and one case of infection progressing to a chronically infected non-union.19 The latter two studies did not describe the management of non-union following LCP.17,19
Neither Meneghini et al. nor Kyriakidis et al. reported the aetiology of non-union following RIMN or LCP, but both described the management.23,25 Following RIMN, Meneghini et al. reported one case being managed with revision to LCP and one with a bone stimulator. The seven cases of non-union after LCP cited in Meneghini et al. were managed as follows: four with revision LCP and bone grafting, two converted to distal femoral arthroplasty and one managed conservatively.23 All three cases of non-union reported in Kyriakidis et al. (one post-RIMN and two post-LCP) were managed with revision total knee arthroplasty.25
Infection was a rarely reported complication after both RIMN and LCP. Aldrian et al. reported one superficial wound infection post-LCP that was successfully treated with antibiotics.16 Horneff et al. reported five cases (one post-RIMN and four post-LCP) and Matlovich et al. one post-RIMN case of infection, that all required surgical management.18,22 Meneghini et al. and Hou et al. both reported a case of infection progressing to chronically infected non-unions, following RIMN and LCP respectively.19,23 As discussed above, Hou et al. also reported a surgical infection post-RIMN eventually necessitating amputation. Finally, Hou et al. described a surgical infection post-LCP that was managed successfully non-surgically.19 Although infection was a rare complication, it had significant consequences with seven of the eleven reported cases requiring surgical management and two cases progressed to chronically infected non-unions.18,19,22,23
Besides non-union and infection, hardware failure/irritation was the third common cause of re-operation. There is clearly significant overlap between cases of hardware failure and non-union, as the former often precedes the latter, as described in all seven cases of non-union post-LCP by Gondalia et al., both cases of non-union post-LCP by Hou et al. and the single case of non-union post-LCP described by Lizaur-Utrilla et al.17,19,21 Aldrian et al. also reported four cases of hardware failure preceding non-union: one case of distal screw loosening following RIMN and three cases of plate breakage after LCP.16 Following RIMN, Horneff et al. reported three cases of unspecified hardware failure and Matlovich et al. described three cases of distal screw irritation, all of which required surgical intervention.18,22 Horneff et al. also described one case of re-fracture after RIMN necessitating surgical re-intervention.18
Femoral PPFs are associated with significant mortality: reported as 17.7% at one year post-operatively by Shields et al. and comparable to the mortality rate after a hip fracture by Bhattacharyya et al.9,29 This meta-analysis found a lower mortality rate of 5.5% for distal femoral PPFs, although the follow up length was variable. Five studies reported on a total of fourteen mortalities. Aldrian et al. reported two mortalities from cardio-respiratory insufficiencies following RIMN.16 Hou et al. reported three mortalities after RIMN and six after LCP, all within six months of surgery and from non-fracture related causes.19 Kilucoglu et al. reported one mortality from pulmonary embolism, on post-operative day one following RIMN.20 Finally, Matlovich et al. reported two deaths post-LCP: one on post-operative day five due to congestive cardiac failure and the other on post-operative day one hundred and eleven following complications from a prolonged stay in the intensive care unit.22
There is limited and conflicting literature comparing native to periprosthetic distal femoral fractures. For example, Streubel et al. reported shorter survival in the PPF group (p = 0.005) whilst Kaufman et al. found no significant difference in mortality (p = 0.55).30,31 Bhattacharyya et al. reported femoral PPF to have a mortality rate comparable to that after a hip fracture, but they did not make any comparison to native distal femoral fractures.29 Further high-quality research is required to draw any substantial conclusions on this comparison.
Six studies reported some data on PROMs using a total of nine different scoring systems.16,17,20,21,24,25 There was no one scoring system used commonly across all six of these studies. Only two of these studies had pre-operative baseline scores to compare to.22,24 The heterogeneity of PROMs data collected across these six studies meant no meaningful conclusion could be made about PROMs after RIMN and LCP for distal femoral PPF.
Whilst this meta-analysis contributes to the growing literature that there is no significant difference in complication rates of RIMN and LCP for distal femoral PPFs; the management strategy is a multi-factorial decision, requiring consideration of fracture pattern, implant stability, co-morbidities of the patient, bone stock and design of the in-situ TKR.32 Non-operative management of supracondylar distal femoral PPFs yields less favourable results than operative management, particularly with regards to non-union and malunion.33–36 Culp et al. reported rates of non-union and malunion as 43% for non-operative management and 13% for operative management.37 However, non-operative management may be the only option for a patient with unacceptably high anaesthetic risk and may be considered in undisplaced epicondylar fractures, provided there is regular follow up to assess for fracture union and preservation of stability.32
For displaced fractures with stable implants, operative fixation is recommended. Historically this involved non-locking plates with dynamic condylar screws,38 which provided improved rates of union compared to non-operative management but often caused significant morbidity due to the extensive incisions and considerable soft tissue stripping.33,34,39 Minimally invasive modern surgical techniques such as RIMNs and LCPs have reduced these complications and there is increasing data to suggest that the outcomes and rates of complications between RIMN and LCP are equivocal.26,27 Deciding between RIMN and LCP often comes down to surgeon preference and experience, but one must consider a handful of contraindications to RIMN. The nail must facilitate safe insertion and recognised contraindications preventing this include: the presence of a patella baja, a closed box design of the in situ TKR and an ipsilateral hip arthroplasty with a long femoral stem which may prevent nail insertion or risk the creation of a stress riser.
Distal femoral PPFs with unstable femoral components require revision arthroplasty or distal femoral replacement (DFR), depending on the quality of bone stock, as outlined in our treatment recommendation flowchart below (Fig. 6). Two recent meta-analyses by Wadwa et al.40 and Ponugoti et al. have reported no significant difference between DFR compared to open reduction and internal fixation (ORIF: a combined cohort of patients who either underwent RIMN or LCP) in rates of complications, re-operation and mortality.40,41 Wadwa et al. also described comparable functional outcome scores between DFR and ORIF, but better post-operative range of motion in the ORIF group.40 These studies also highlight the advantage of early mobilisation and weight bearing post-DFR, reducing length of hospital stay and immediate sequela of immobility. This is supported by Tandon et al., who reported shorter length of hospital stay and lower complication rate (19% vs 40%) following DFR when compared to ORIF.42 These initial findings are encouraging but further research is necessary to illuminate the overall risks and outcomes of DFRs for distal femoral PPFs.
This meta-analysis is not without limitations. There is a scarcity of high-quality data that underpins the topic of distal femoral PPFs. Nine of the ten studies included in this meta-analysis, were retrospective cohort studies that lacked randomisation. There are limited case numbers involved in these studies and both aetiology and management of complications are variably reported across studies, further reducing quantity of data and the statistical power of the subsequent analyses. Surgeon preference greatly influences choice of fixation method and is a multi-factorial decision, influenced by experience with each technique, institutional trend, fracture pattern and bone quality. Fracture pattern was both variably reported and not standardised across the ten studies. Without this information, we were unable to elucidate what contribution fracture pattern had in deciding surgical technique and any potential influence on rates of complications.
Conclusion
This meta-analysis finds no significant difference in rates of non-union, re-operation, infection, or mortality between LCP and RIMN. At present, the framework provided, offers recommendations for the management of distal femoral PPFs. Further high-quality research is essential to evaluate both poorly reported outcomes, and emerging treatment modalities in the future.
Abbreviations
Arbeitsgemeinschaft für Osteosynthesefragen (AO)
Orthopaedic Trauma Association (OTA)
Distal femoral replacement (DFR)
Intramedullary (IM)
methodological items for non-randomised studies criteria (MINORS)
National Joint Registry (NJR)
NICE (National Institute for Health and Clinical Excellence)
Open reduction and internal fixation (ORIF)
Periprosthetic fracture (PPF)
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)
Total knee replacements (TKRs)
United Kingdom (UK)
United States of America (USA)

_flow_diagram_o.png)

.png)





_flow_diagram_o.png)


.png)




