I/ INTRODUCTION
Patients suffering from irrecoverable radial nerve palsy (RNP) experience not only the inability to extend their wrist and fingers but also a significant reduction in hand grip strength by up to 77%.1 In cases of non-recovering RNP, tendon transfer is considered the optimal approach. Author Merle D’Aubigné.2 selected the pronator teres muscle for transfer to the extensor carpi radialis longus and extensor radialis brevis, the flexor carpi ulnaris muscle to the extensor digitorum communis and extensor pollicis longus, and the palmaris longus to the abductor pollicis longus and extensor pollicis bevis. However, several authors.3–6 argue that the flexor carpi ulnaris muscle is the strongest and more crucial wrist flexor compared to the flexor carpi radialis muscle. Transferring the flexor carpi ulnaris muscle for extensor digitorum communis can lead to wrist joint radial deviation deformities and decreased grip strength. To overcome these limitations, authors suggest utilizing the flexor carpi radialis muscle as the dynamic finger extensor due to its greater muscle length and minimal influence on the wrist joint axis. Additionally, transferring the pronator teres muscle to both the extensor carpi radialis longus and extensor radialis brevis is unnecessary as it exacerbates wrist joint radial deviation deformities. Therefore, authors advocate transferring the pronator teres muscle solely to the extensor radialis brevis to minimize wrist joint radial deviation.3,7–10 Based on these perspectives and after reviewing the literature, I have chosen the modified Merle D’Aubigné tendon transfer method: transferring the pronator teres muscle to the extensor radialis brevis, and the flexor carpi radialis muscle to the extensor digitorum communis and extensor pollicis longus, along with the palmaris longus muscle to the abductor pollicis longus and extensor pollicis bevis. This approach has not been studied in practical treatment in Vietnam. This is the rationale for conducting the research titled “Treatment of Irrecoverable Radial Nerve Palsy using the Modified Merle D’Aubigné Tendon Transfer Method” with the objective of assessing the outcomes of treating non-recovering motor RNP using the modified Merle D’Aubigné tendon transfer method.
II/ MATERIALS AND METHODS
Patients over 16 years of age, regardless of gender, admitted to the Department of Plastic and Reconstructive Surgery, Hospital for Traumatology and Orthopaedics, between January 2017 and December 2018 were included.
Inclusion Criteria: Patients with a confirmed diagnosis of non-recovering radial nerve palsy (RNP) or prognosis of irrecoverable RNP, eligible for tendon transfer when: RNP persisted for over 6 months without signs of recovery, patients over 55 years of age with RNP were not suitable for primary repair, RNP cases with concomitant extensive soft tissue injuries and abdominal muscle involvement, where prognosis for direct repair was unfavorable, patients expressing the desire for tendon transfer surgery and were in an appropriate health condition.
Exclusion Criteria: Patients lacking the palmaris longus. Patients with combined ulnar nerve and median nerve injuries, injuries involving muscles not selected for dynamic transfer, muscles selected for dynamic transfer had muscle strength ratings of 3 or lower on the British Medical Research Council (BMRC) scale, stiffness in the wrist and hand joints, limited passive range of motion before tendon transfer surgery, inadequate bone healing, calcified ligaments or narrowed joint spaces, soft tissue defects or scars along the tendon pathway and unrepaired joint defects.
Study Methodology: The study utilized a prospective longitudinal design. The evaluation criteria were based on the following five measures (assessed using Tajima T’s classification).11: Degree of joint motion recovery, extent of wrist joint radial deviation deformity, recovery of grip strength compared to the unaffected side, overall functional recovery assessment, patient satisfaction level with surgical outcomes.
Data Collection and Processing: Data were collected using information collection forms and analyzed using t-tests. Statistical analysis was performed using Stata 14.0 software.
III/ RESULTS
Between January 2017 and March 2019, a total of 33 patients underwent tendon transfer surgery using the modified Merle D’Aubigne method. The mean follow-up period was 13.2 ± 7.3 months. The male-to-female ratio was 32:1, with males constituting the majority at 97%. Home accidents were the leading cause (45.46%), followed by traffic accidents (33.33%). The incidence of left limbs and right limbs injuries were nearly equal, with 16 left limbs and 17 right limbs. The ratio of non-recovering radial nerve palsy (RNP) to non-recovering posterior interosseous nerve palsy (PINP) was 16:17. The mean time from injury to surgery was 7.8 ± 10.8 months, ranging from a minimum of 4 months to a maximum of 60 months.
The average wrist extension angle was 48.6° ± 14.9° when extending the fingers and 30.9° ± 14.4° when flexing the fingers. The average wrist flexion angle was 34.8° ± 15.8° when extending the fingers and 42.6° ± 14.8° when flexing the fingers. 93.9% of patients could fully extend their fingers when the wrist joint was extended beyond 10°. The average thumb abduction angle was 55.3° ± 7.4°. The Kapanji score averaged at 8.4 ± 1.2. The surgery did not induce wrist joint rotational deformity. 32 out of 33 patients (97%) expressed satisfaction with the surgical outcomes, and 31 out of 33 patients (94%) returned to their original professions.
The mean age was 29.1 ± 10.8, with the lowest being 17 and the highest being 59 (Table 1).
In most cases, initial treatments included simple wound closure with or without bone fixation (23/33 = 69.69%). 9 out of 33 cases (27.28%) involved initial examination and management of nerve injuries (Table 2).
Twenty five out of 33 patients (75.76%) achieved active wrist extension beyond 30° when flexing the metacarpophalangeal joint (MCP joint), with 8 patients (24.24%) achieving extension beyond 50°. The average wrist extension angle when flexing the MCP joint was 42.6° ± 14.8 (Table 3).
In 20 out of 33 cases (60.61%), grip strength exceeded 60% compared to the unaffected side. The average grip strength was 65.4% compared to the unaffected side (Table 4).
The results presented in Table 5 demonstrate that 31 out of 33 cases (93.9%) achieved Excellent or good outcomes, with 2 out of 33 cases (6.1%) achieving fair results and no cases demonstrating poor outcomes.
IV/ DISCUSSION
Wrist Extension Recovery
In this study, we employed the pronator teres tendon as the driving force and transferred it to the shortened extensor carpi radialis brevis. The average wrist extension angle when flexing the fingers was 42.6° ± 14.8°. This result is comparable to that of Pham Hoang Lai’s study.,7 which reported 39.4° ± 17.6°. According to Altintas AA.,10 the average wrist extension angle was 44° ± 6°. Ropars M.12 indicated an average wrist extension angle of 38°. Al-Qattan MM9 reported an average wrist extension angle of 45 degrees. The wrist extension angles in our study align with those reported by authors who similarly restored wrist extension motion by transferring the pronator teres tendon to the extensor carpi radialis brevis. Timothy D.6 also emphasized that transferring the pronator teres tendon to the extensor carpi radialis longus can contribute to radial deviation deformity of the wrist joint. Douglas MS.5 highlighted that currently, despite various tendon transfer techniques, transferring the pronator teres tendon to the extensor carpi radialis brevis is a widely adopted approach.
Recovery of Finger Extension
In our study, the flexor carpi radialis muscle was utilized for restoring finger extension movement. The results indicated that 93.9% of patients had the capability to fully extend their fingers when the wrist joint was extended beyond 10°. This finding is in line with the outcomes reported by Pham Hoang Lai.,7 which demonstrated 91.8%. The average finger extension angle at the metacarpophalangeal joint in our study was 15.1° ± 7.1°, which is higher than that reported by Pham Hoang Lai.7 at 9.7° ± 2°. This discrepancy is due to our deliberate adjustment of tendon tension during the transfer of the flexor carpi radialis tendon to the extensor digitorum communis.
The calculation of finger extension angles among various authors lacks uniformity. Al-Qattan MM9 documented an average deficiency in finger extension angle of 4°. Ishida O.13 recorded an average finger extension angle of 5° for the third finger (with the wrist extended by 30°). Nonetheless, we noted that authors utilizing the flexor carpi ulnaris tendon for restoring finger extension often reported radial deviation deformities of the wrist joint. Altintas AA’s study.10 employed both the method of using flexor carpi radialis and flexor carpi ulnaris for restoring finger extension. The authors reported an average wrist radial deviation angle of 190° ± 60°. They also suggested that Merle D’Aubigne’s tendon transfer method should be modified because in patients with posterior interosseous nerve paralysis, wrist extension movement is still predominantly governed by the extensor carpi radialis longus muscle. In such cases, the flexor carpi ulnaris should be selected for tendon transfer. Should the flexor carpi ulnaris tendon be chosen, the radial deviation deformity of the wrist joint would become more pronounced.
Shamar YK.14 used the flexor carpi ulnaris tendon for restoring finger extension. The author noted that all patients with posterior interosseous nerve paralysis (13 cases) in the study had wrist radial deviation deformities, with an average deviation of 14°. The author attributed this deformity to the utilization of the flexor carpi ulnaris tendon as the dynamic force, despite its potential for passive correction. According to Timothy D6, using the flexor carpi ulnaris tendon for finger extension recovery can result in wrist radial deviation deformities. This condition may be exacerbated if the pronator teres tendon is transferred to the extensor carpi radialis longus for wrist extension recovery. Therefore, the authors recommend considering the contraindication of using the flexor carpi ulnaris tendon in patients who have preoperative wrist radial deviation deformities and those with posterior interosseous nerve paralysis.
Douglas MS.5 stated that although the flexor carpi ulnaris tendon was one of the initial choices for tendon transfer, nowadays surgeons prefer the flexor carpi radialis muscle and the flexor digitorum superficial. This preference is due to the loss of wrist flexion function caused by the removal of the flexor carpi ulnaris. Additionally, patients with paralyzed extensor carpi ulnaris can experience wrist imbalance and radial deviation deformities of the wrist joint.
Restoration of Thumb Movement
In our study, flexor carpi radialis tendon was transferred to the pollicis longus and the extensor digitorum communis, passing through the interosseous membrane. To restore thumb abduction movement, we applied the method proposed by Merle D’Aubigne, utilizing the palmaris longus tendon threaded beneath the skin, transferred to the abductor pollicis longus, and then extensor pollicis brevis. At this point, the palmaris longus tendon not only functioned for thumb abduction but also supported thumb extension. The average thumb abduction angle in our study was 55.3° ± 7.4°, closely resembling the findings of Pham Hoang Lai.7 (58.6° ± 8.4°) and surpassing the results of other authors such as Altintas AA10 (46° ± 10°) and Shamar YK.14 (44°).
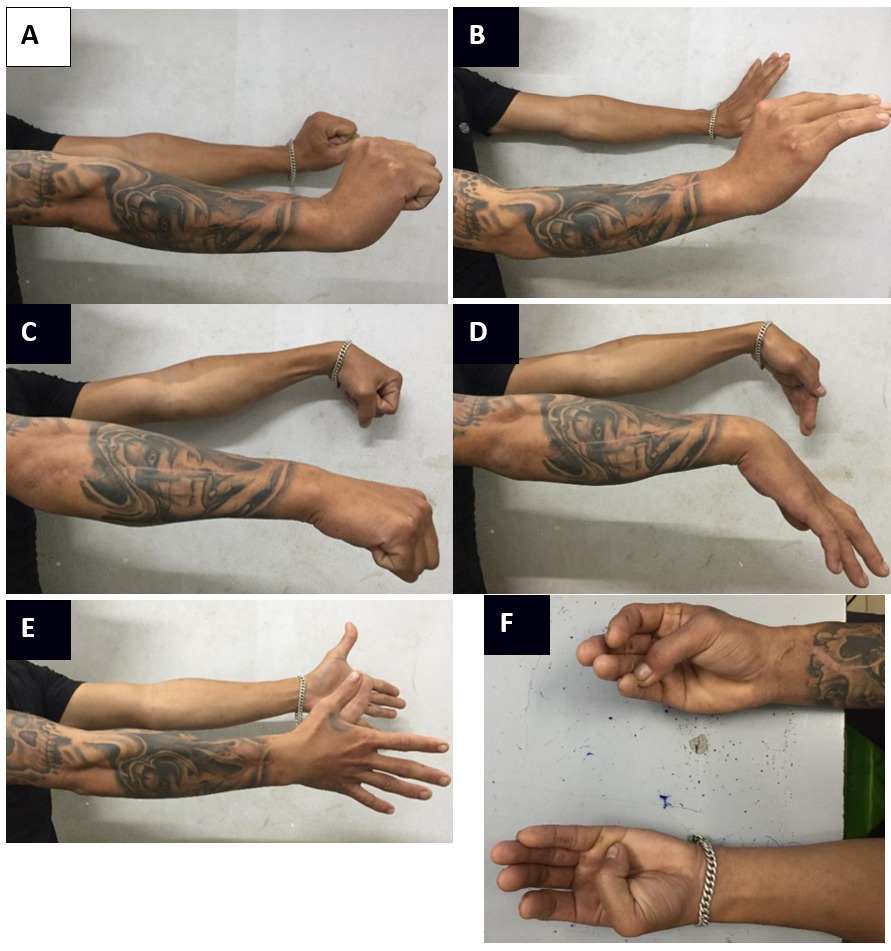
Clinical examinations conducted several months after surgery (Figure 1) revealed that the majority of patients could independently perform thumb abduction compared to the long fingers. This is attributed to the simultaneous contraction of the abductor pollicis longus and extensor pollicis brevis when the palmaris longus contracts. According to Kruft S.,15 this technique helps maintain the thumb in a neutral position, preventing constriction between the thumb and index finger under the pull of the adductor pollicis muscle, thereby enhancing the opposition movement of the thumb. The average Kapanji score achieved in our study was 8.4 ± 1.2, higher than the result of Shamar YK14 (7.8).
Restoration of Grip Strength
The average achieved grip strength in our study was 65.4% compared to the unaffected side, closely resembling the findings of Pham Hoang Lai.7 at 70% and surpassing the results of other authors using other methods. In cases of radial nerve palsy, due to the paralysis of the extensor muscles, the wrist joint is passively flexed when fingers are flexed. Therefore, grip strength is significantly affected. Labosky DA1 reported a 77% reduction in grip strength in cases of radial nerve palsy. Following the transfer of tendons to restore wrist extension, hand grip strength is substantially regained. In cases of low radial nerve palsy, where the extensor carpi ulnaris and sometimes the extensor carpi radialis brevis are paralyzed, grip strength is also affected but to a lesser extent.
Al-Qattan MM.9 performed tendon transfers to treat RAP and PINP in 15 patients, resulting in postoperative hand grip strength reaching 46% compared to the unaffected side. Altintas AA.,10 using both the Brooks and the modified Merle D’Aubigne tendon transfer methods on 77 patients, achieved an average postoperative hand grip strength of 51% compared to the unaffected side. Skoll M.12 treated 22 patients using the flexor carpi ulnaris tendon as the motive force for finger extension, resulting in grip strength of 52% in RAP cases and 62% in PINP cases.
In conclusion, the use of the flexor carpi radialis tendon for tendon transfer while preserving the flexor carpi ulnaris tendon helps maintain the functional axis of the wrist joint. As a result, grip strength restoration is superior to the method of using the flexor carpi ulnaris tendon as the motive force.
Overall Results
In our study, 29 out of 33 patients (87.8%) achieved excellent results, 2 out of 33 patients (6.1%) achieved good results, 2 out of 33 patients (6.1%) achieved fair results, and no patient had poor results. Additionally, 32 out of 33 patients were satisfied with the surgical outcomes, and 31 out of 33 patients were able to return to their previous occupations. These results closely resemble the study by Pham Hoang Lai7 involving the treatment of non-recovering RAP through the Smith tendon transfer method. In that study, 80.3% achieved excellent results, 18.1% achieved good results, 1.6% achieved fair results, and all 60 out of 61 patients were able to continue with their previous occupations. Al-Qattan MM9 noted 80% of patients achieved excellent results and 20% achieved good results. Altintas AA10 also reported that 89% of patients were able to return to their previous occupations. According to Shamar YK.,14 68% of patients achieved results ranging from good to excellent, 32% had fair results, and no patients had poor results.
The treatment of non-recovering radial nerve paralysis through the modified Merle D’Aubigne tendon transfer method yields excellent outcomes. The utilization of the pronator teres tendon transfer for extensor carpi radialis revis is highly suitable. The group of patients with radial nerve palsy (n=16) displayed an average wrist extension range of 37.9° ± 14.1° when flexing the fingers and 32.1° ± 17.8° when extending the fingers. This modification has been researched and recommended by numerous authors worldwide. Implementing the flexor carpi radialis tendon transfer for extensor digitorum communs, including the extensor pollicis longus, constitutes a rational adaptation. This approach was well-suited for 31 out of 33 patients (93.9%) who achieved full finger extension range when the wrist joint was extended beyond 10°, and it did not lead to radial deviation deformity of the wrist joint. The range of motion of the thumb and the long fingers was nearly restored to normal. The average grip strength achieved was 65.4% compared to the unaffected side.
Ethical approval
Approved at our institution.
Funding
None.