Summary
-
Acromioclavicular joint dislocation is considered a common injury among athletes.
-
Previous studies agreed to state the non-surgical management for low grade Rockwood injuries (Type I-II), where surgical management is reserved for high grade injuries (Type IV-V).
-
Treatment of type III AC separation has been debatable for the last decades.
-
Most of the recent literature suggested starting non-surgical treatment for type III and considering surgical treatment if pain or instability persisted.
-
The only exception is high-performance athletes where surgical treatment is advised to be considered initially.
Epidemiology
Acromioclavicular (AC) joint separation is defined by a loss of articular contact between the distal end of the clavicle and the medial part of the acromion.1 It is characterized by a disturbance in the stabilizing ligaments (AC ligaments and Coracoclavicular (CC) ligaments).1 AC joint separation represents around 10% of all other shoulder girdle injuries. The affected populations are usually young athletic males in their 20s to 30s of age.2 Nearly half (40-50%) of these shoulder injuries occur during contact sports 3,4 And associated shoulder injuries were found in 18% of the patients.2,5
Mechanism of injury
AC joint separation is mainly caused by either a blunt injury to the superolateral aspect of the shoulder or secondary force by a fall on the outstretched hand or elbow with a superiorly directed force, during contact sports.2 While the shoulder is in adduction, a direct blow to the acromion can lead to systematic failure starting with failure of the AC ligament with the capsule initially, then failure of the CC ligament and last is deltotrapezial fascia. The magnitude of ligament injury is directly correlated with the force of the injury.4
Anatomy
The AC joint is a diarthrodial joint between the medial side of the acromion and the distal clavicular articular surface. This joint connects the shoulder to the axial skeleton. AC joint harmonizes three joint movements concurrently including glenohumeral, scapulothoracic, and sternoclavicular joints.3 Each joint has a static and dynamic stabilizer. Similarly, the AC joint the static stabilizer plays the most important role in the stability of the AC joint which includes AC ligaments and capsule.4 The primary horizontal plane stabilizers are superior and posterior AC ligaments, whereas the primary vertical stabilizers of AC joint are Conoid and Trapezoid ligaments (CC ligaments).4 Dynamic stabilizers play a secondary role in the AC separation which consists of anterior fibers of the deltoid muscle that are attached to the clavicle and trapezius muscle via fascial that is inserted into the acromion.4 The most predominant blood supply to the joint comes from the axillary artery (through the thoracoacromial branch) and subclavian artery (through the suprascapular branch).4
Presentation
AC Joint injury is easily missed, therefore any patient who presents with shoulder trauma and complains of pain around the AC joint, AC separation must be suspected. On clinical examination, it should be performed in both sitting and position with keeping the arm not supported. Downward force can exacerbate the deformity making it more obvious.4 The findings of the clinical examination vary based on the severity of the injury and the presence of surrounding injuries. The patient typically presents with their injured side elbow supported by the contralateral hand. With more severe trauma, skin manifestations in the form of swelling and ecchymosis may be present. Skin tenting and/or blanching should alert impending open injury and soft tissue compromise. Almost all patients, present with tender acromioclavicular joint. Shoulder range of motion (ROM) is usually not affected, but some patients can present with limited shoulder ROM due to discomfort only. Further stress test can help in the clinical diagnosis of AC separation such as cross-arm adduction and loading of the AC joint which can be helpful in milder grade injuries as a reference to the AC joint pathology. Although neurovascular injury is rare in these injuries, it is mandatory to rule out brachial plexus or vascular injuries due to the nature of the location of the AC joint that is surrounded by vital structures. Other injuries are reported to a lesser extent such as (intra-articular extension and lung involvement in the form of pneumothorax) which should be ruled out with higher energy injuries.3
Diagnostic Imaging
Plain radiographs are required for diagnosis, including a true Anteroposterior view (AP), in addition to the Velpeau view (beam aiming 45 degrees cephalic) and Zanca view (15 degrees cephalic tilt). Other views are required to rule out other injuries such as AP shoulder and axillary views. A contralateral side radiograph is required and considered to evaluate the patient’s normal CC distance. The role of advanced imaging is limited in AC separation.6 Magnetic Resonance Imaging (MRI) of the shoulder can further delineate the integrity of the ligaments, accurate grading of the injury, and presence of arthritic findings in the AC joint and it can accurately identify associated injuries.7 In certain studies, it was reported that MRI can provide an upgraded injury of AC separation.7 MRI is not the standard for diagnosis of AC separation but may be useful in low-grade injuries.7 The AC injury in MRI is demonstrated in the form of high signal intensity in T2 images.8 Computed Tomography (CT) gives a further description of AC separation if associated with fractures, but for isolated AC separation, the role of CT is equivalent to plain radiographs.6
Classification
A grading system was designed to describe the severity of injury based on the number of disrupted ligaments and the resultant clavicle displacement was made by Rockwood.9 He classified the injury into 6 types and his classification is widely used nowadays (Table 1). Type I represents a sprain with intact AC and CC ligaments and clinically demonstrates minimal or no tenderness and normal radiographs. Type II is characterized by a horizontal axis instability with an increased CC distance by <25% of the contralateral side. AC ligament considered in this type partially disturbed. Type III presents with complete disruption of both AC and CC ligaments (unstable on the horizontal and vertical axis with CC distance increased 25-100% compared with the normal side). Type III injuries have been subdivided into IIIA with pure vertical instability and IIIB with additional horizontal instability. Type IV is considered a unique type where the clavicle is posteriorly displaced and entrapped through the trapezius muscle. Significant superior migration and translation of the clavicle is classified as Type V (CC distance >100% of contralateral side) whereas inferior displacement, sometimes even subcoracoid, of the clavicle is classified as Type VI.9
Management
Non-operative management
Non-surgical management is the treatment of choice for Types I and II which takes the form of protection and immobilization using an arm sling to minimize stress on CC and AC joints.10 The duration of immobilization for type one is 7 to 10 days whereas for Type II immobilization may last 4-6 weeks to help in the improvement of the patient’s symptoms.10 The rehabilitation program starts immediately after immobilization and resolution of the patient’s symptoms.11 It starts initially with a passive and active-assisted range of motion (ROM).10 Whenever the patient achieves full ROM, isometric strengthening exercises should start, followed by isotonic exercises. Return to sports that is involved with body contact and weightlifting has to be after 8-12 weeks from injury.10,12
Operative management
Surgical intervention is indicated in all acute AC dislocations for Types IV, V, and VI since it carries severe injury to surrounding tissues.13 The literature contains much debate regarding surgical versus non-surgical management for Type III injuries.4 The primary goal of surgical intervention is to reduce and maintain the AC joint anatomically.13 Multiple surgical fixation techniques were previously reported in the literature and can be classified based on the method to: Acromioclavicular (AC) fixation, Coracoclavicular (CC) fixation, dynamic muscle transfer, and ligament reconstruction.10 The initial management of acute injury Type III has been the subject of much controversy. Most studies advocate the nonsurgical option for Type III, although some support surgery for acute injuries in young patients, patients whose job places high demands on the shoulder, or high-performance throwing athletes. Many clinicians also draw the distinction between the presence of concomitant horizontal instability (confirmed clinically and/or radiographically) and recommend surgical treatment for type IIIB injuries. Type III patients who were treated initially with conservative management and presented with persistent/chronic pain or instability may also benefit from the surgical option (relative indication), Although there is no conclusive evidence for this in the reviewed studies.
The ISAKOS Upper Extremity Committee recently suggested treating Type III injuries non surgically, but in case of persistent pain or it starts to affect the patient’s ability to return to sports activities or work duties for more than one-month, surgical options should be considered. In addition, a Meta-analysis done by Phillips et al showed comparable overall satisfactory rates for Type III injuries whether treated surgically or non-surgically. Patients who were managed non-surgically exhibited early return to work and prior injury activities while surgically treated patients had a relatively high complication rate, but the clinical outcomes of both treatments were comparable.14 Both surgical and non-surgical options were shown to provide equivalent outcomes in terms of prevention rate from osteoarthritis, persistent pain and clinical scores.14 Though, the chronic AC pain was to a lesser extent in the surgically treated group. In contrast, a systematic review revealed multiple advantages and disadvantages associated with nonoperative management. Which includes shorter rehabilitation intervals and the absence of hospitalization. The downsides were the possibility of a moderate degree of chronic pain, AC joint instability, decreased shoulder movements, and if reconstructive surgery is needed later, it will be technically difficult since the clavicle has been displaced for a long duration, and would most likely require soft tissue augmentation to the primary repair. Despite it is noticed the low rate of persistent AC pain for the patients who underwent surgery, the current data are inadequate to establish a scientific conclusion regarding the differences between surgical and nonsurgical treatment concerning the functional outcome and patient satisfaction. A well designed Randomized Controlled Clinical Trials (RCT) are necessitated to establish a well-structured treatment plan for Type III injuries.
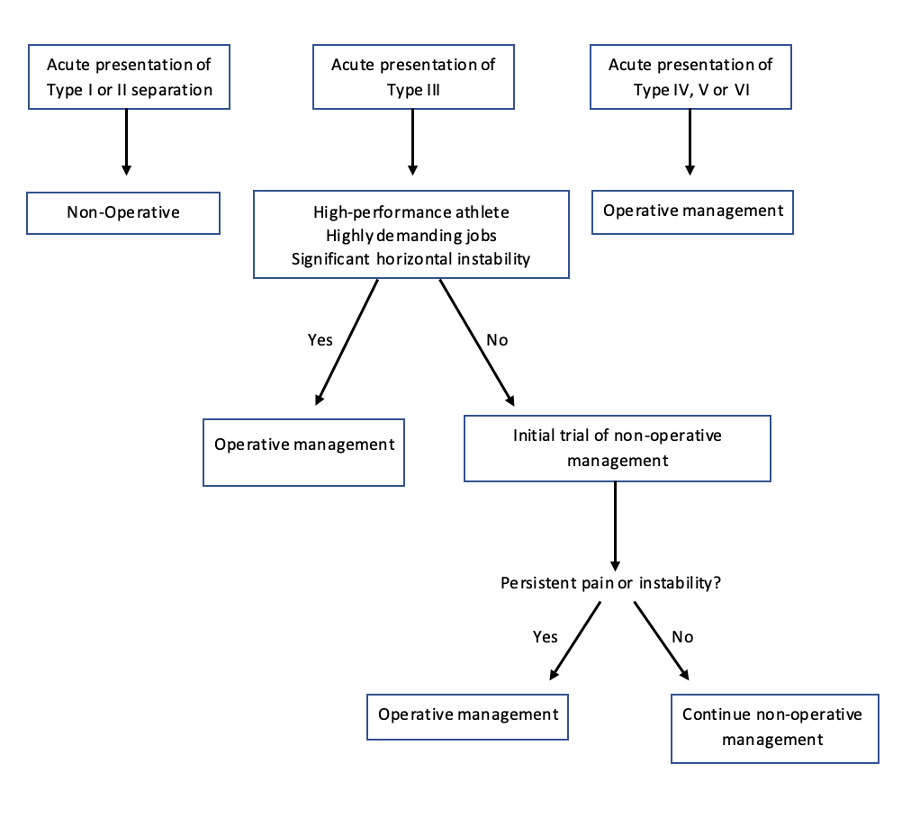
For the success of the nonsurgical treatment of higher-grade AC separations, a proper and adequate rehabilitation program is essential. The usual regimen consists of an arm sling for one to one and a half months followed by a supervised physiotherapy protocol which includes a passive and active range of motion of the shoulder, followed by muscle resistance exercises, and strengthening one and a half months after the injury. To avoid early stiffness, surgeons can instruct their patients to start pendular exercises anytime from the trauma incident. Strengthening should include the muscles of the shoulder girdle including deltoid, trapezius, sternocleidomastoid, and subclavius muscles. Rotator cuff muscles and the periscapular stabilizer muscles have to be included in the strengthening phase of the rehabilitation program. A summary of reported treatment results and recommendations for AC separation grade III is described in Table 2. An algorithm designed by the authors for the proposed treatment for Type III AC separation is in Figure 1.
Methods of surgical fixation
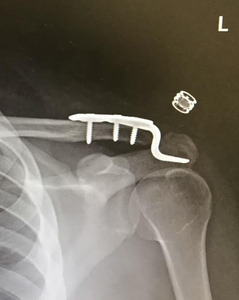
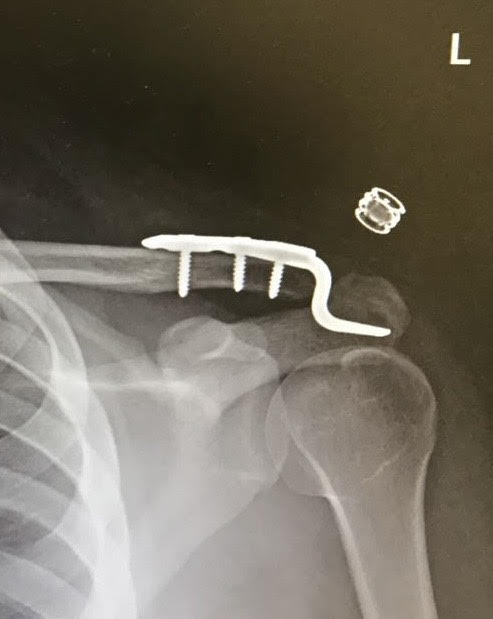
Primary fixation of AC joint
Acromioclavicular fixation was first described using smooth Kirschner wires or threaded wires.10 This technique was restricted due to the disastrous complications including the risk of injuring vital structures such as great vessels, lungs, and heart.10 Another technique that was described and has become much more common nowadays is hook plate fixation, which is considered less invasive (Figure 2).17,18 The hook plate is designed to be fixed with multiple screws over the superior aspect of the lateral end of the clavicle, where it curves a in Z-shape so the medial part of the plate can slide underneath the acromion to provide upward resistance to the clavicle.10 The hook plate fixation can be done alone, or it can be augmented with ligament reconstruction.17 The hook plate requires a period of immobilization until the ligaments have healed.18 The hook plate is considered a strong and stable construct, but it is associated with early and late complications, thus removal of the hardware after healing is recommended.11,17
Coracoclavicular fixation
This technique aims to reduce AC joint through coracoclavicular (CC) fixation.10 The leading idea was by Bosworth using a screw starting from the clavicle and directed to the coracoid but has been associated with potentially dangerous complications.13 Numerous papers describe different techniques with the same principle of fixation including the CC suture button (Figure 3).10 This method is preferred in terms of less need for further surgeries and hardware removal compared with hook plate fixation.13 CC suture button can be achieved by either utilizing single or double clavicular buttons with a loop around the coracoid.13 This method carries unique complications including suture cutout or clavicle osteolysis.10 Suture buttons are reported to be comparable biomechanically to native ligaments.11 Screw fixation or CC suture button mostly combined with CC ligament reconstruction as recommended by Rockwood to increase the stability.10
Ligament reconstruction
The first description of the use of the native coracoacromial ligament to reconstruct Acromioclavicular joint injury was by Weaver-Dunn.10 It is performed by resecting the lateral end of the clavicle and using the bony acromial end of the coracoacromial ligament to supplement the resected part of the clavicle. The idea of this technique is to utilize the CA ligament as a substitute for the CC ligament.11 This technique is no longer commonly used due to the high failure rate (30%) and low biomechanical stability in correlation to the CC ligaments.11 A modification in the technique has been described which aims to reconstruct CC ligaments with autogenous semitendinosus graft, or allograft and mechanically support of the construct either through CC button fixation or hook plate fixation.11 The modified Weaver-Dunn technique can be carried out in an open fashion or using the arthroscopic technique, as described by Lafosse.10 Arthroscopic ligament reconstruction is considered less invasive and may provide better visualization.13
The use of allograft carries a higher failure rate in terms of radiographic outcome compared to autograft.21 Autograft is reported to be biomechanically superior to CA ligament reconstruction of CC ligament.17 It can be performed by passing a loop of the graft beneath the coracoid process, then securing both ends to the clavicle either by creating two parallel bone tunnels or simply tying the ends over the intact clavicle.17
Dynamic muscle transfer
This technique aims to transfer the coracoid process with its tendons including the short head of biceps, coracobrachialis, and pectoralis minor where it gets fixed to the distal end of the clavicle to help in vertical stability.10 It is first described by Dewar and Barrington.23 Wang et al. combined the dynamic muscle transfer technique with the use of the hook plate in 21 patients which showed a satisfactory outcome among the majority of patients.24 Due to the high rate of complications including coracoid process fracture and musculocutaneous nerve injury, this technique has been abandoned.10,24
Clinical outcome
Non-surgical management
Literature about the outcome of non-surgical management for Types I and II AC separation is limited, but Pallis et al have shown around 10% of those AC injury groups who were treated initially with nonsurgical management underwent subsequent surgery.25 Mohsin et al, found half of the low grade AC separation patients were asymptomatic during follow-up.21 Recent literature suggests non-surgical management for Type III in acute AC separations specifically for older age and patients who aren’t committed to high-demand jobs or sports activities.10 It is reported that conservative management is effective for Type III patients who are professional baseball players.10 Non-surgical management may alter shoulder mechanics which may lead to shoulder dyskinesia, decreased bench press strength, or may affect sports strength.10
Surgical management
The outcome of surgical management has been studied for single techniques or combined techniques. Alexander et al. studied the radiological outcome for patients presented with Rockwood types III, V and treated with hook plate fixation and have shown that 12% of cases experienced a postoperative loss of reduction.18 In a study where they compared the functional outcome of open or arthroscopic suture buttons with hook plate fixation, the suture button demonstrated a favorable functional outcome and better pain score.26 Furthermore, the arthroscopic suture button showed superior functional outcomes compared with the open technique.26 Müller et al reported athletes who underwent arthroscopically assisted double-suture-button experienced a return to sports ability and normal sports activity level compared with athletes who underwent open hook plate fixation.10,27 Gunnar et al compared the outcome of combining arthroscopic tight rope fixation augmented with hook plate in 69 patients, both techniques showed good to excellent clinical outcomes, comparable partial recurrence in CC distance with a complication rate of almost 13% for both groups.28 However, Weihui et al concluded that the tight rope technique is better in functional recovery, pain scale, less operative time, less loss of reduction, and CC distance.29
Ligament reconstruction has become one of the most used techniques nowadays. Mazzocca et al biomechanically studied different types of techniques comparing anatomical CC ligament reconstruction with two bundles of semitendinosus autograft, arthroscopic reconstruction with high tensile braided polyethylene suture, and a modified Weaver-Dunn procedure.30 Anatomical reconstruction with autograft is the closest biomechanically to normal AC and CC ligaments.30 In metanalysis comparing arthroscopic with open reconstruction, a comparable rate is noticed in terms of failure of reduction, complications and the need for further surgeries.31 Comparing clavicular tunnels in ligament reconstruction, double tunnels carried a higher rate of complications including clavicle fracture.32 Allograft carries a higher risk of the need for revision surgeries, whereas autograft has a higher failure rate of reduction.32
Postoperative failure of the reduction was described in the literature after open reconstruction or arthroscopic suture button fixation. The risk of this complication can range from 17% to 80%, however partial or residual displacement has not been shown to precipitate functional deficit.16,33-35 Although it can be technically challenging, arthroscopic assisted AC repair or reconstruction has the possible advantages of direct judgment of the reduction and the assessing the need to address additional shoulder pathologies as concomitant injuries may occur in up to 25% of patients.36,37 Arthroscopic approach is considered relatively a safe procedure in multiple case series but well-designed RCTs are needed to compare the outcome of this intervention to open techniques.
Timing of surgery is another consideration as early surgical intervention tends to be easier and leads to accurate reduction of the joint in comparison to delayed surgery. Song et all review showed better reduction and clinical outcome when surgery is performed in less than 3 weeks but without significant difference in the complication rate.38
Management of chronic AC injury
Chronic AC dislocation has historically been described as more than 4-6 weeks from injury.39 Management of high-grade chronic AC separations is considered a challenge, due to the loss of healing potential of torn CC ligament compared to acute AC separation that needs anatomical reduction.40 For that reason, biological augmentation should be considered in the management of chronic AC separation.40 The Modified Weaver Dunn technique is described in the management of chronic AC separation but carries lower resistance in vertical stability compared with reconstruction with tendon graft.40 Tauber et al showed a better outcome in cases where anatomical reconstruction was performed using semitendinosus tendon autograft compared with those who underwent the modified Weaver Dunn technique.41 A comparison has been studied of modified Weaver Dunn technique augmented with Polydioxanone (PDS) and hook plate fixation alone, patient who underwent open reduction and fixation with hook plate experienced higher pain scores during shoulder range of motion and at rest, whereas ligament reconstruction group experienced good shoulder range of motion and better satisfaction.42 A systematic review compared multiple different techniques in chronic AC separation showed the best functional outcome noticed among patients who underwent anatomical reconstruction with the use of both synthetic and biologic augmentation.43
Complications
Complications after AC separations may occur after non-operative and operative treatment, and can include pain, stiffness, deformity, and weakness.10 In general, the complication rate among the surgical group was around 27 to 44%.36 One of the most common complications is a complete failure of reduction or partial loss.21 Hardware complications, including the need for removal of the hardware, and the presence of infection are the most common complications associated with surgery. The general complication rate of the hook plate technique is around 11%.44 While infection alone can present in 5% of those patients.45 In patients where the plate is retained for a long time, acromion osteolysis or fracture can happen at a higher rate. In a cadaveric study, the location of the contact point joining the lateral tip of the plate over the inner surface of the acromion was variable among specimens. That finding was mainly attributed to the wide surface area of acromion. Males tend to have wider and thicker acromion compared to females.46 Clavicle and coracoid fractures are reported complications in the techniques that utilize a bone tunnel.21 This can be prevented if the graft is wrapped over the clavicle or coracoid rather than creating bone holes that predispose to fracture.21 The incidence reaches up to 5.3% and it is correlated with the width of the tunnel.21 Hardware migration to great vessels can happen with old techniques.10 The end result is early AC arthritis, persistent instability, or clavicle osteolysis which is presented in the form of persistent AC pain and tenderness.10,17
Conclusion
A greater recognition of the approach and management of Acromioclavicular joint separation has been growing for the last few decades. Many treatment options have been evolved and reported in the literature for this injury. It has been known that the proper management for acute low-grade AC separations (Type I, II) is conservative, whereas the standard treatment for high-grade acute AC separations (Type IV - VI) is surgery. Most of the persistent debate is on finding out the optimal management for type III injuries. We present the most updated review of the management of Type III AC separation. The latest consensus evidence suggests starting initially with conservative management for acute Type III injuries for most patients including contact sports athletes. Where surgical management should be considered if there is significant horizontal instability or if the patient is a high-performance athlete, e.g. throwing athlete, and if initial non-surgical management leads to continuous non-responsive pain and/or instability.
Competing interests
No conflict of interest between authors:
Funding, grant/award info
None.
Data availability
No applicable
Acknowledgement
N/A
Authors contribution
Waleed Albishi: Research idea, research design, designing algorithm.
Fahad Alshayhan: Literature review, writing the article, submission of the article.
Afnan Alfridy: Literature review, writing the article.
Abdulrahman Alaseem: Literature review, writing the article.
Amr Elmaraghy: Final review edit, designing an algorithm.