INTRODUCTION
The American College of Rheumatology defines osteoarthritis (OA) as a heterogeneous group of disorders that cause joint symptoms and indicators linked to defect articular cartilage integrity and ultimately result in "joint failure1,2 It was considered a degenerative joint disease resulting from wear and tear. Nowadays, it’s the complex combination of biomechanical and mechanical insults that exceeds the joint’s ability to repair itself.1 OA affects about 3.3 to 3.6% of the population globally. It causes moderate to severe disability in 43 million people, making it the 11th most debilitating disease worldwide.3,4 In 2016, the enormous disease burden caused by OA led to the Osteoarthritis Research Society International (OARSI) submission of a White Paper, describing OA as a Serious Disease.5,6 There are many predilection sites for OA, such as knee, hip, hand, etc, but the most common one is the knee and hip respectively.
Knee osteoarthritis (KOA) as one type of arthritis, that especially occurs in the elderly, yet the incidence shows an increasing trend at an alarming rate. It has become a great burden of disability, pain, and socioeconomic cost worldwide.7 After the age of 60, women (13%) are more likely than males (10%) to develop symptomatic KOA.7 Pain, one of distinct features of KOA, is the most common symptom for a patient who decides to visit health care and is prior to disability.8 First-line pharmacological therapy to treat OA is a Non-steroidal anti-inflammatory drug (NSAID); chronic use of NSAID leads to many systemic side effects such as gastrointestinal bleeding, hepatotoxic, and other.9
One of other treatment modalities for KOA is intra-articular injection. This method is preferred since it has less or almost none systemic effects. One of the most popular solutions nowadays is Hyaluronic Acid (HA) and Platelet Rich Plasma (PRP). Hyaluronic acid is identical to a substance that synoviocytes produce. Hence , it works like a lubricant and shock absorber in the joints.10 Platelet-rich plasma (PRP) is a portion of whole blood acquired by centrifugation of autologous blood to separate and extract the plasma and portion of the blood, resulting in high concentrations of platelets.11 Thus, PRP contains a higher concentration of platelet-derived growth factors (PDGFs) than autologous platelets.12 Platelets facilitate tissue repair through degranulation from alpha granules, which involves the release of PDGF, vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), basic fibroblastic growth factor (bFGF), and transforming growth factor-β1 (TGF-β1).13
The purpose of this study was to compare the outcomes between intra-articular injection of hyaluronic acid and Platelet-rich plasma in knee osteoarthritis by using several indicators such as EuroQOL-visual analog scale (EQ-VAS), visual analog score (VAS), Western Ontario Mcmaster Osteoarthritis Index score (WOMAC score), International Knee Documentation Committee (IKDC) score, and Tegner score
METHOD
The present study was performed in accordance with the guideline by Cochrane Collaboration Research of Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) checklist to improve transparency.14,15 We chose the modified Jadad scale to ensure the quality of the literature we picked.16 The writer also used Assessment risk of bias using the Cochrane Risk of Bias 2 (RoB2) Tool.17,18
Search strategy
This study conducted a thorough search of published literature to find a complete, peer-reviewed paper on evaluating intra-articular injection of HA versus PRP for KOA by two independent reviewers (G.I and Y.A). In case of disparity, two reviewers solved it through a discussion. The literature was searched through PubMed, Science Direct, and Google Scholar using Boolean operators with the following keywords: “Knee Osteoarthritis” or “Knee OA” and “Hyaluronic Acid” or “HA” and “Platelet-rich Plasma” or “PRP” and “Randomized Controlled Trial”.
Inclusion and exclusion criteria
Inclusion criteria for this study are: (1) Study Design: included pRCTs of KOA treated with intra-articular HA and PRP. (2) Study Participants: Individuals diagnosed with KOA, either clinically or radiographically, regardless of their gender, age, or race. (3) Study Intervention: group intervention included intra-articular HA or PRP. (4) Study Outcome Measures: At least one of the predetermined outcomes that were reported: WOMAC, EQ-VAS, VAS, IKDC, Tegner score, and other indicators.
The exclusion Criteria for this study including: (1) Non-RCT literature. (2) Duplicate published literature. (3) Studies on which the data could not be extracted.
Quality of literature
A modified Jadad scale was used to assess the quality of the literature. Several criteria include randomization, blinding, withdrawals, dropouts, inclusion/ exclusion criteria, adverse effects, and statistical analysis.16 The sum for every literature score from 0 to 8. The score 0 to 3 indicated low-quality studies, whereas scores 4 to 8 indicated high-quality studies.9 The consensus was achieved by a process of deliberation and agreement over the selection of literature that may offer the most robust evidence, given the available facts at the time
Assessment risk of bias
The Cochrane Risk of Bias 2 (RoB2) Tool which consists of five domains which about randomization process, Deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Then, the sum of five domains then labelled into low-risk, some concern, and high-risk bias.17,18
RESULT
Literature search and selection
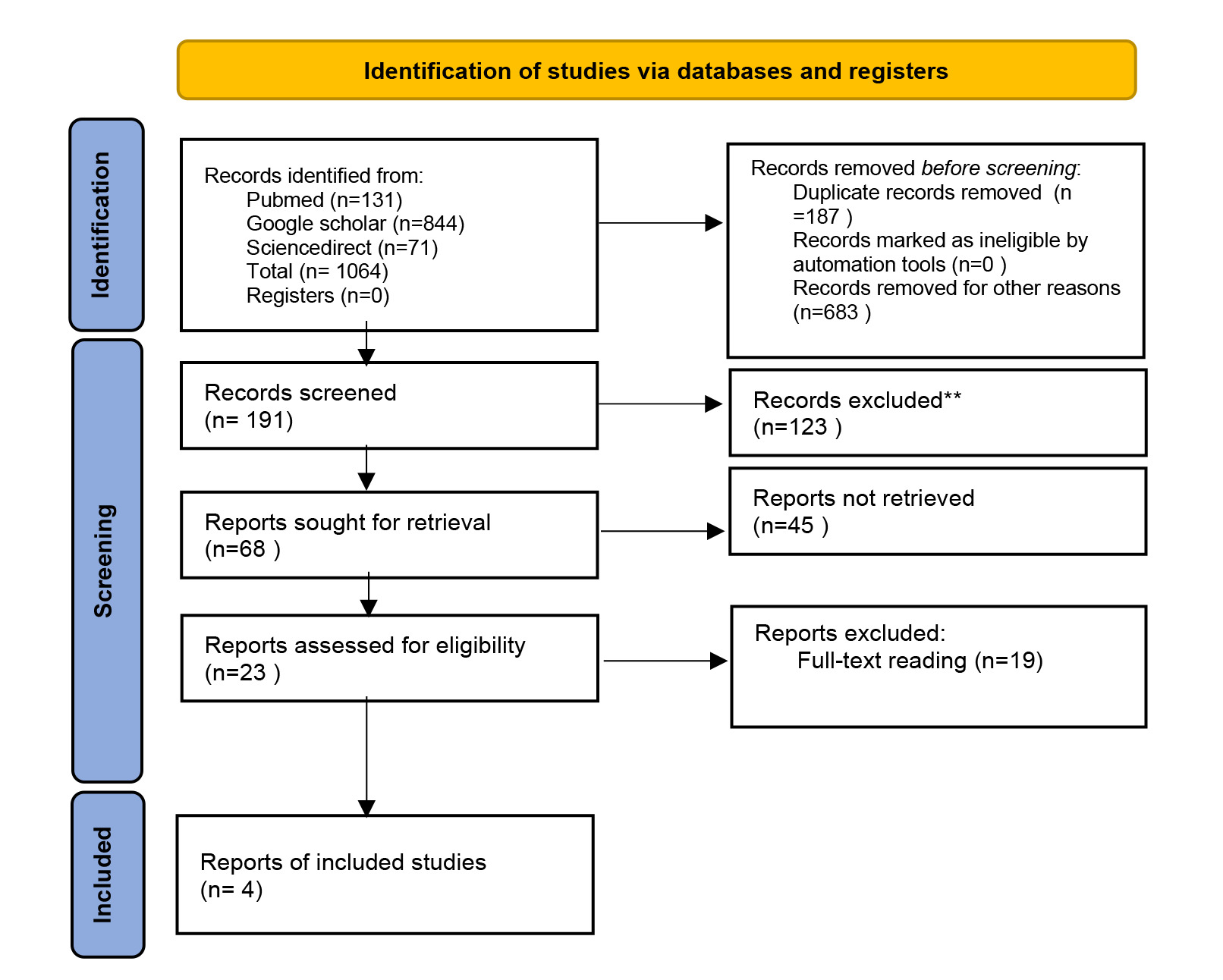
We screened to report relevant results based on inclusion and exclusion criteria which were downloaded full articles that met the criteria and underwent data extraction. As seen on Figure 1, among 1064 studies found using our search strategy, 187 were excluded based on duplication. Additional 683 studies were excluded based on title screening, and further 123 studies were excluded after reading the abstract. The remaining 23 studies were reviewed, and the final article included in this review was 4 studies.
Characteristic of literature
The characteristics of the 4 literature can be found in Table 1. Total number of patients included in this study is 447, 198 were treated with PRP, and 194 received HA. All literature was published between 2018 and 2022, among these four studies, all are pRCTs.
Quality
Upon assessing the literature through a modified Jadad scale, one of the studies by Tavassoli et al. achieved the highest score, mentioning both inclusion and exclusion criteria.
All studies have the similarity of lacking an approach to assess adverse effect criteria. Nevertheless overall, all studies were recorded to have scored above 4, interpreted as high-quality studies as seen on Table 2.
Risk of Bias
RoB-2 tools were used to assess the risk of bias in included literature. Domain one assessed concerns regarding randomization, and four studies (100%) were rated as low risk of bias. All studies (100%) were rated as low risk of bias in domain 2, which is regarding deviation from intended intervention, and also rated as low risk of bias in domain 3, which is regarding missing outcome data.
All studies in domain 4 about measurement of the outcome rated as low risk. One study in domain 5 assessed the selection of the reported result was regarded high risk of bias, the rest is either low risk (50%) or some concerns (25%). Overall, two studies are regarded as having a low risk of bias, one is high risk of bias,and the other possesses some concerns as seen on Figure 2 and Figure 3.
Outcome
The available research have consistently demonstrated that both PRP and HA treatments result in substantial improvements for KOA as evaluated using several indicators including WOMAC, EQ-VAS, IKDC, VAS, and Tegner scores. Three studies using WOMAC score as an indicator for functional improvement. Two of them reported significant decrease in WOMAC score in PRP group compared to HA group, and one study by Wang et al. reported no significant differences in WOMAC score between PRP and HA. Two studies by Martino et al. and Lin et al. observed PRP group showed significant reduction in IKDC Score compared to HA group
Overall, among the four trials that were examined, the findings from three prospective studies by Wang et al., Martino et al., and Lin et al. indicated that there was no difference in patient reported outcome observed between the groups receiving PRP and HA. In contrast, the study conducted by Tavassoli et al. reached the conclusion that PRP demonstrates a considerably superior efficacy compared to HA in the treatment of KOA, with a statistically significant difference.
DISCUSSION
Osteoarthritis, the most common form of chronic progressive arthritis, especially in the knee, accounted for immense pain, disability, and economic burden. The etiology and pathogenesis are multi-factorial, its thought as a resultof biomechanic and or mechanical process that exceeds cartilage’s capabilities to regenerate itself.1 First-line treatment of mild-moderate KOA (Kellgren-Lawrence ≤3 or Ahlback ≤3) includes lifestyle modification and NSAID to relieve pain.19
Chronic usage of NSAIDs led to many adverse systemic side effects such as gastrointestinal problems, etc. Hence current alternative trend is to administer intra-articular solutions such as HA and PRP to provide relief.20–23
Since the application of intra-articular injection of HA and PRP has soared in the last decade, it is crucial to understand the mechanism and efficacy of both. For this study, we use only high-quality randomized controlled trials, which we assess using modified Jadad score. We also assess the risk of bias from the aforementioned studies using the ROB2 tool.
All the studies showed that both PRP and HA yield significant improvement for KOA assessed by several indicators such as WOMAC, EQ-VAS, IKDC, VAS, and Tegner scores. On the other hand, out of four studies we reviewed, the data based on three prospective studies showed no significant comparison between PRP and HA groups.20–23 In contrast, Tavassoli. Et al. concluded that PRP is significantly better than HA (P<.001) for treating KOA. His study also stated that the highest efficacy of PRP was observed in both groups at week four, with about 50% decrease in the symptoms compared with about 25% decrease for HA, and stated that PRP efficacy increases after multiple injections.23 This correlates with studies from Lin et al. that showed PRP clinically significant functional improvement for at least 1 year of therapy.22 Martino et al.also revealed that the re-intervention rate at 24 months was significantly lower in the PRP group (22.6% vs 37.1%, P=.036).21 We observed that duration of therapy seems to play role in PRP usage. For long-term usage, PRP seems to be superior to HA. However there is insufficient data for objective outcome improvement for PRP uses in KOA.
Several differences were observed from all studies that may interfere with the outcome. First, the preparation of PRP and HA. PRP which is acquired from the centrifugation of autologous blood to separate the plasma and blood components, acts as a vector for many growth factors.24 Other literature stated that growth factor contained in PRP promotes tissue repair, which is more aligned with OA pathogenesis.25 Numerous methods can be used to prepare a PRP solution, yet there needs to be more standardization on how to prepare it. Many ways can be used to achieve a higher concentration of average platelet, as higher platelet concentration is associated with a higher concentration of growth factor.24,26 All studies we reviewed aimed for leucocyte-poor PRP with different methods.20–23 The double-spin method is recommended to prepare PRP to achieve higher concentration of average platelet compared to the single-spin method.24 Two studies (Tavasolli and Martino et al.) used the double-spin method. However, there is a slight difference in rpm and minutes. Meanwhile, two other studies (Wang and Lin et al.) used single-spin method. Platelet activator using 10% calcium chloride was also used in one of the studies by Martino et al.. Activation of PRP is not required when injected into soft tissue as the natural collagen type I acts as a natural activator.24 The science behind the ideal preparation of PRP is still in research. We only found two of our studies that stated their PRP checked for quality tests.
On the other hand, HA, one of the most essential components of synovial fluid, plays a role in lubricating the joints.25 Several clinical studies demonstrated that HA has the effect of relieving joint pain, thus reducing disability. The latest guidelines for KOA did not recommend HA as a primary therapy, which possesses no impact on cartilage regeneration.27 Other than that, HA is regarded as symptomatic therapy unrelated to the underlying pathogenesis of KOA, and studies from stated that the effectiveness of HA decreases after multiple applications.25,28 HA is provided by several manufacturers which vary in molecular weight. Based on the data from four studies defined the use of high molecular weight HA (HMWHA) for the treatment of OA. HWHA defined as a molecular weight above 1.000kDa.25 HMWHA is preferred to low mollecular weight HA (LMWHA) because, the latter has an ability to act as a pro-inflammatory up-regulation, promoting the activation and maturation of dendritic cells, releasing pro-inflammatory cytokines such as interleukin1 beta (IL-1β), tumor necrosis factor α (TNF-α), IL-6, and IL-12. Besides that, it also increased the expression of chemokines and promoting cell proliferation.29,30
The number of injections also varied among these studies, including single injection, and multiple injections which were repeated at different times. One study by Tavasolli et al. also compared single injection vs double injection of PRP, resulting in double injection being better than single injection or HA treatment (WOMAC total score 61.57±11.29 vs 63.71±9.87).
Beyond those differences in this study, the mechanism of PRP and HA in the change of KOA was an essential factor that may influence the outcome. The therapeutical effects of HA may be attributed to improved lubrication. Growth factors in PRP are fundamental to stimulate the proliferation and differentiation of chondrocytes, regulate collagenase, and thus regenerate the cartilage.31 The combination of HA and PRP may be more beneficial than alone. Another study concluded that the combination of HA and PRP resulted in better outcomes than HA alone for up to one year and PRP alone for up to three months.32
Nevertheless, few limitations were inexorable. First, the follow-up time was relatively short, and PRP and HA’s long-term efficacy and safety could not be evaluated. Second, only one study used NS as a placebo hence we cannot determine whether the PRP and HA given had a placebo effect. Third, the amount of PRP (mL) differs in each study ranging from 4 mL to 5 mL. Lastly, in terms of grading the OA, some studies use KL grading, and the rest use Ahlback grading, which may affect the credibility of effectiveness.
CONCLUSION
We concluded that intra-articular injection of HA or PRP could improve the total WOMAC, IKDC, VAS, and Tegner score however, there is uncertainty regarding whether the PRP is superior to HA since there was no standardized procedure for preparing PRP solution, which can affect the results. Other than that, there is no consensus regarding the dosage of PRP injected. Also, all the indicators used were very subjective. Hence we can not conclude that PRP affected cartilage repair. In the future, some objective indicators including MRI to assess cartilage or pathological studies will be essential to be included in the outcome assessment.