1. Introduction
A hip replacement is a major surgery indicated for many hip joint conditions such as hip joint degeneration, avascular necrosis of the femoral head, or femoral neck fractures. Understanding the morphology of the hip joint helps surgeon in performing the surgery more accurately. On the other hand, hip morphology is different between human races and geographical regions.1,2 The comparison of the anatomical feature of the hip joint between human races and geographical regions is developing in parallel with the trend of personalized treatment for the patients.
With the advancements in medical imaging technology, it has become feasible to meticulously plan surgical procedures using multislice computed tomographic system (CT) with multiplanar reconstruction (MPR). Besides individualized clinical evaluation, MPR of CT allows measurement of the parameters of the acetabulum as well as the orientation of the acetabulum in 3D space, thereby, contributing to successful surgical outcomes. Preoperative measurement of morphological parameters of the acetabulum opens the door to advancements in the development of artificial substitutes that are tailored to individual patient parameters.
Because several earlier studies have provided a characterization of the anatomical feature of the hip joint, our study aimed to evaluate several anatomical parameters of the shape, size, and spatial orientation of the acetabulum in adult Vietnamese patients with indications for the total hip arthroplasty based CT with MPR.
2. Materials and Methods
2.1. Study Design & Patients
After obtaining approval from the Institutional Review Board of the Hanoi Medical University, we prospectively analyzed a total of 63 acetabula in 35 consecutive patients who received indications for the total hip arthroplasty in the Department of Orthopaedic Surgery and Sports Medicine of the E Hospital (Hanoi, Vietnam) from January 2021 through December 2022.
2.2. Measurement Performance
We use the 64 Slice Siemens SOMATOM Perspective CT Scanner with model DC045D from Germany for imaging. Patients are scanned in a supine position and balanced on the scanner table, with their legs in an intermediate position and their knees extended straight at 0 degrees. Imaging parameters: the field of view (FOV) width ranges from 300-400 mm; the voltage is between 110-140 kV; the current intensity is 100 mAs; the slice thickness is 0.6-1 mm; the reconstruction interval is 1-1.2 mm for bone window and the software on the coronal, axial, and sagittal planes; and the table feed is 0.8-1.2 mm.
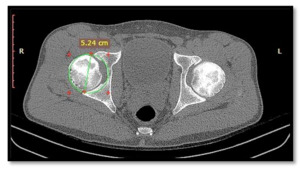
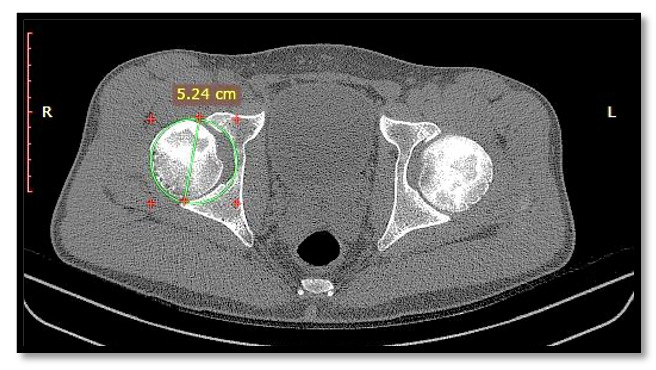
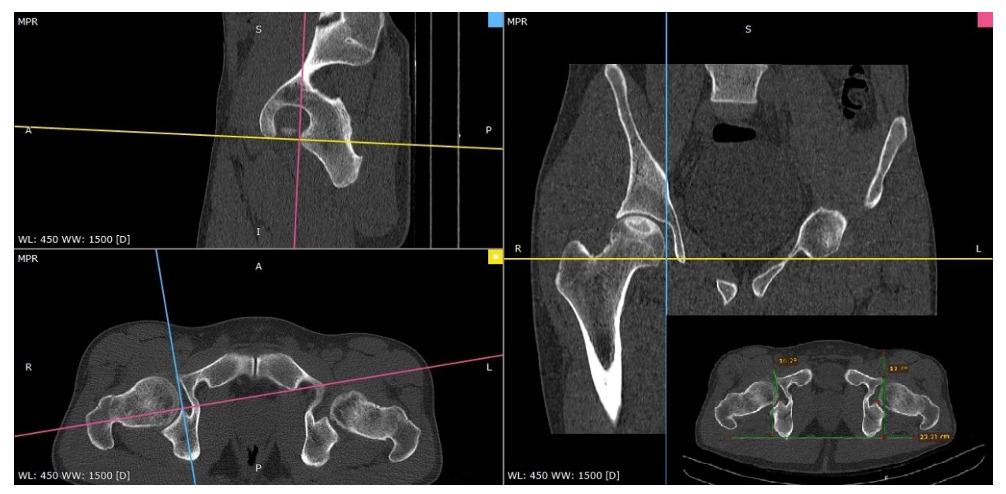
On CT with MPR images, circular designs encompassing the entire acetabulum are created at the position with the largest dimensions to measure the diameter of the acetabular opening (Image 1). On coronal images, the depth of the acetabulum is measured as the distance between the deepest point of the acetabulum and the line connecting the “tear drop” to the outermost point of the acetabulum (Image 2). The acetabular depth ratio is calculated as the depth of the acetabulum divided by the length of the line connecting the “tear drop” to the outermost point of the acetabulum, multiplied by 1000.
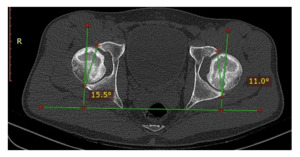
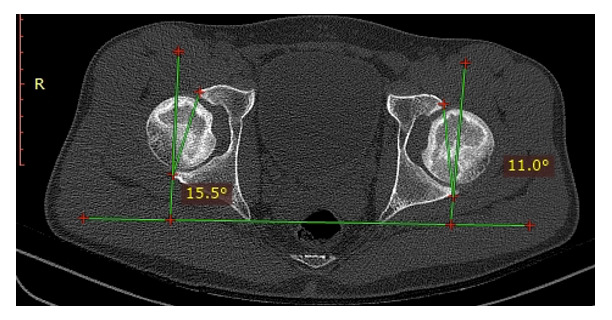
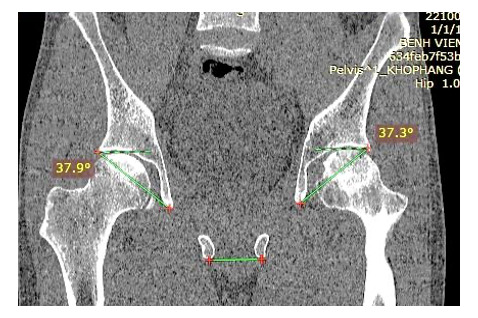
The acetabular anteversion angle was measured on the axial plane as the angle formed by the line connecting the anterior and posterior edges of the acetabulum with the line perpendicular to the line connecting the two ischial tuberosities (Image 3). The acetabular inclination angle was determined on the coronal plane as the angle formed by the line connecting the superior outer edge of the acetabulum and the “tear drop” with the horizontal line passing through the two ischial tuberosities (Image 4).
The horizontal offset index of the hip joint is determined on the coronal plane as the distance from the center of the femoral head to the “tear drop” landmark (Image 2). The sagittal acetabular angle is determined on the sagittal plane as the angle formed by the line connecting the anterior and posterior rims of the acetabulum and the horizontal plane (Image 5).
Regarding the orientation of the transverse acetabular ligament, on CT with MPR, we determine the posterior horn of the acetabular notch on the axial plane, then adjust the orientation bars on both the axial and sagittal planes until the anterior horn of the acetabular notch is identified on both planes. Then, the angle of anteversion of the transverse acetabular ligament on the axial plane is measured, which is formed by the line connecting the anterior and posterior horns of the acetabular notch and the line perpendicular to the connecting line of the two ischial tuberosities (Image 6).
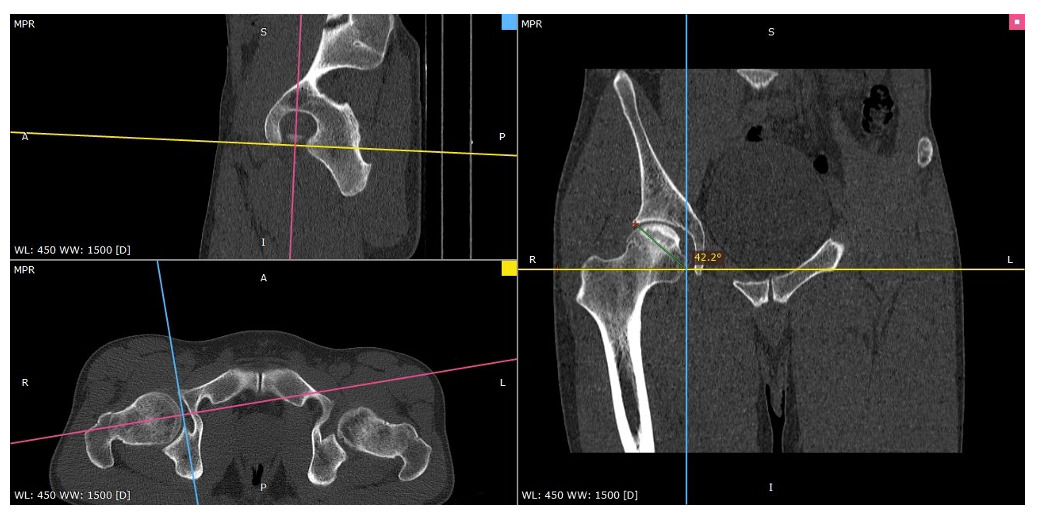
The inclination angle of the transverse ligament is determined on the CT with MPR, by moving the center of orientation of the plane to the midpoint of the line connecting the anterior and posterior horns in the axial and sagittal planes. At this position, the center of orientation is also located at the midpoint in the coronal plane. The inclination angle of the transverse ligament is defined as the angle between the horizontal reference line and the line connecting the center of orientation to the outer superior margin of the acetabulum (Image 7).
2.3. Statistical Analysis
Parameters were measured using Radiant Dicom viewer software. The data obtained was entered in EpiData 3.1, and responses were coded appropriately before being exported to Stata® 15 (StataCorp LLC, College Station, TX, USA) for analysis. The data was expressed as mean ± standard deviation (SD). The morphological features of the acetabulum were compared between genders using either the Mann-Whitney U test or the t-test. The Pearson and Spearman correlation coefficients (r) were utilized to evaluate the relationship between the values of the morphological features of the acetabulum and the body mass index. Several selected relationships between morphometric parameters of acetabulum were illustrated with Scatterplots. p-value <0.05 was considered to be statistically significant.
3. Results
The analysis included a total of 63 acetabulum (29 right acetabulum & 34 left acetabulum) in 35 patients. There were 25 males (71.4%) and 10 females (29.6%). Mean age was 56.35±13.15 years (Min-Max: 18-79). Mean BMI was 23.4±2.9 kg/m2 (Min-Max: 18.4-30.1).
There was no statistically significant difference between men and women according to the angles describing the orientation of the acetabulum (Table 1).
Table 2 showed the statistically significant difference between genders in AHO (p<0.001) and acetabular diameter (p<0.001).
Correlations amongst morphometric parameters of acetabulum were revealed in Table 3.
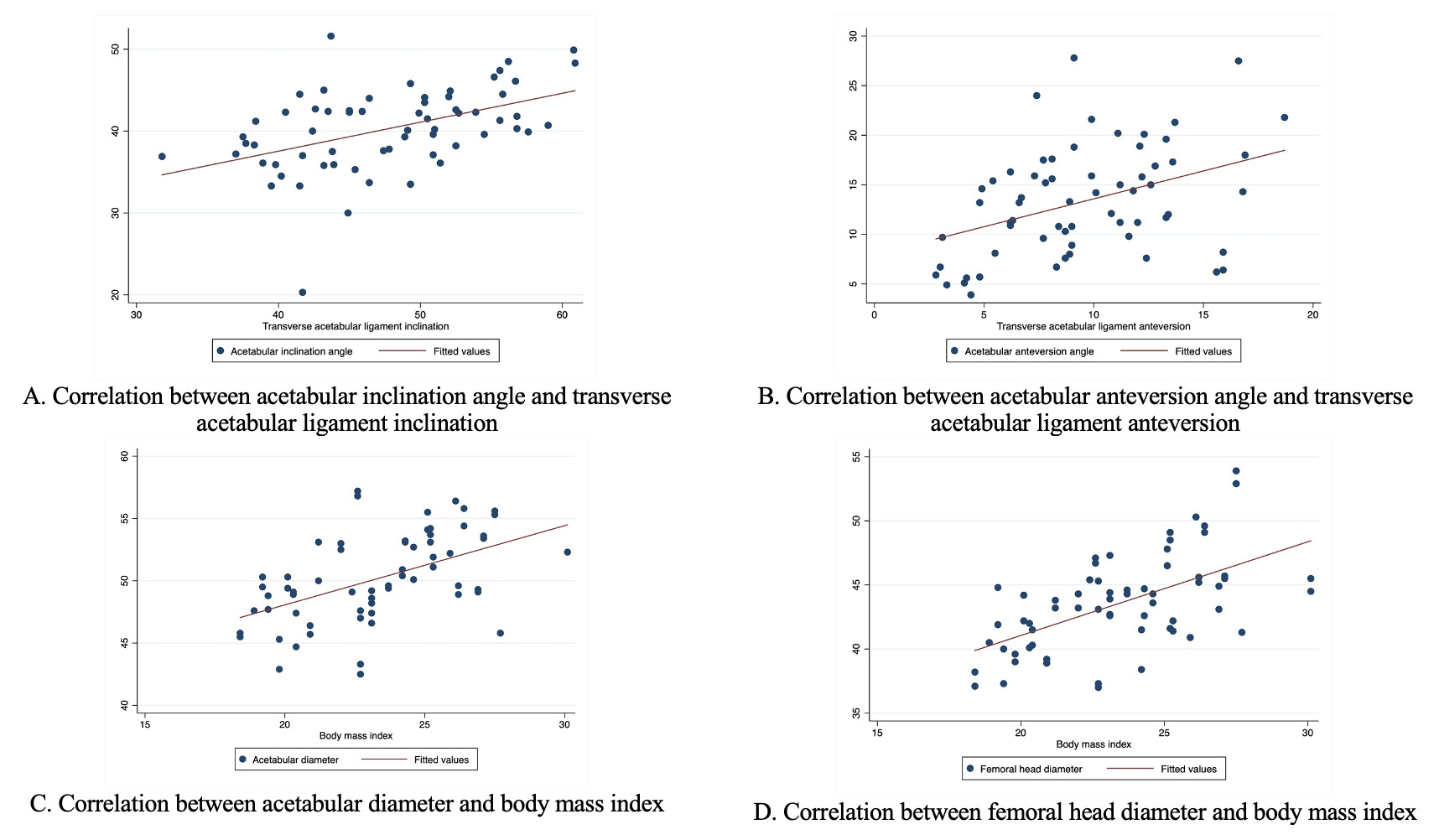
Table 4 showed correlations between body mass index and morphometric parameters of acetabulum. BMI was negatively correlated with AAA (r: -0.2928) and SAA (r: -0.3003), while BMI was positively correlated with AHO (r: 0.5340) and Acetabular diameter (r: 0.5183). Several selected relationships between morphometric parameters of acetabulum were revealed in Figure 1.
4. Discussion
The differences in the anatomical morphology of the hip joint in general and the acetabulum in particular among different human races need to be clearly understood to ensure precise surgical planning.1,3 In addition, with the trend towards personalized surgical instrumentation (PSI), accurate measurement and orientation of the acetabulum prior to surgery facilitates the selection and fabrication of instruments and implants that are appropriate for the size of each patient. In our study, the average size of the acetabulum was 50.22 ± 3.5 mm, which is similar to the study by Tran Trung Dung (2019) of 50 ± 2.9 mm, both on a group of mature Vietnamese individuals.4
The depth of the acetabulum and acetabular depth ratio in our study were 18.62 ± 2.95 mm and 309.6 ± 41.87, respectively, compared to Tran Trung Dung’s study (2019)4 which reported 24.3 ± 2.2 mm and 485 ± 37 for Vietnamese adults, and Zeng’s study (2012)5 of the Chinese community, Baharuddin’s study (2018)6 of Malaysians, Paul’s study7 of Indians, and Arsic’s study8 of Serbians, in which no statistically significant difference was found in acetabular depth and index. The average size of the femoral head in our study was 43.54 ± 3.68 mm, which was not statistically different from Tran Trung Dung’s study (2019).4 Regarding the differences in this index between different ethnicities and genders, Edward reported in 2020 that there were statistically significant differences between ethnic groups, especially between the Chinese and white European, white American, and African American populations.2,9–11 In terms of the orientation angles of the acetabulum in space, we compared our results with those of other authors in the literature (Table 5).
A particular structure of the acetabulum is the transverse acetabular ligament (TAL), which has been identified not only as a stabilizer of the hip joint but also as a guide for the placement of artificial acetabular components in total hip replacement surgery. This was confirmed by Archbold in his studies in 200619 and 2008.20 Our study showed the inclination and anteversion angles of the TAL to be 47.7 ± 6.73 degrees and 9.49 ± 3.92 degrees, respectively. We can see the different when compare the TAL orientation angle in our study with previous studies in the Table 6. The difference between males and females is shown in the Table 7.
We can see that there is no difference in the inclination angle between our study and other studies worldwide (Table 7). However, there is a difference in the anteversion angle compared to other studies. Previous studies have indicated that the TAL plays a role in orienting the placement of artificial hip joints. Some studies have found that it is involved in the anteversion angle, while others have found it is involved in the inclination angle. In our study, we found a linear relationship between both the anteversion angle and the inclination angle of the TAL and acetabulum. Therefore, our study suggests that the TAL plays a role in orienting the placement of artificial hip joints for both the inclination and anteversion angles.
5. Conclusions
Measuring the anatomical parameters of the hip joint and acetabulum is a critical step in preoperative planning for hip replacement surgery. This allows the surgeon to understand the patient’s specific anatomical measurements and devise a plan for selecting appropriate tools and the best surgical strategy. The transverse acetabular ligament serves as a visible anatomical landmark during surgery and plays a significant role in guiding the placement of the artificial acetabulum, ultimately resulting in the highest surgical outcome.
Authors’ contribution
Conceptualization, D.-H.N. and T.-D. T.; methodology, D.-H.N., T.-T.N., K.-T.L., S.-T.P. and T.-D. T.; software, D.-H.N. and T.-D. T.; validation, D.-H.N., T.-T.N. and T.-D. T.; formal analysis, D.-H.N., H.-L.V. and T.-D. T.; investigation, D.-H.N., T.-T.N., K.-T.L., S.-T.P., V.-H.D., X.-H.L., M.-D.T. L., H.-L.V. and T.-D. T.; resources, D.-H.N., T.-T.N. and T.-D. T.; data curation, D.-H.N., V.-S.N., H.-L.V. and T.-D. T.; writing—original draft preparation, D.-H.N., H.-L.V. and T.-D. T.; writing—review and editing, D.-H.N., T.-T.N., K.-T.L., S.-T.P., V.-H.D., X.-H.L., M.-D.T. L., H.-L.V. and T.-D. T.; visualization, D.-H.N., T.-T.N., K.-T.L., S.-T.P. and T.-D. T.; supervision, T.-D. T.; project administration, D.-H.N.. All authors have read and agreed to the submitted version of the manuscript.
Fundings
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Hanoi Medical University (No. 468/GCN-HĐĐĐNSYSH-ĐHYHN).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability
The data used in this article are available upon request from the corresponding author. The data are not publicly available due to the protection of personal data.
Acknowledgments
First of all, we sincerely thank the study participants and their family for your help in the measurement of morphological parameters. Also we thank Board of Directors from E Hospital for supporting data collection.
Conflicts of Interest
The authors declare no conflict of interest.
Corresponding author
Professor, Ph.D, MD Tran Trung Dung
Director of Orthopaedic and Sports Medicine Center
Chairman of Orthopaedic Department, VinUniversity
Director of 3D Technology in Medicine Laboratory, VinUniversity
Mail: dungbacsy@dungbacsy.com ; Tel.: +84.983762005