Introduction
The patella is the largest sesamoid bone of the human body and situated on the anterior surface of the knee. The main function of the patella is to transfer the force of quadriceps to tibia to generate knee movements. Patellar fracture is a common scenario in orthopedic clinics, and it usually occurs due to a sudden impact to the patella.1,2
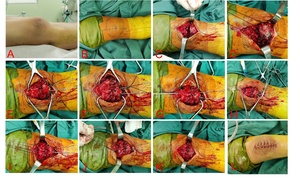
Fractures of the infrapatellar pole are a unique type of patellar fracture in which the patella is extraarticularly avulsed by the patellar tendon. Such fractures account for 5 to 22.4% of all patellar fractures.3 There are multiple surgical techniques available for the treatment of infrapatellar pole fractures. However, it is worth noting that in some cases, patients have reported soft tissue irritation around the knee following surgery. Consequently, a portion of these patients may require subsequent removal of the implant as a secondary procedure.4,5 To address these concerns, alternative surgical techniques have been developed. The purpose of this study is to demonstrate the repair of a displaced infrapatellar pole fracture using the Suture Bridge technique with 5-Ethibond (Fig. 1).
Materials and methods
Patient demographics
A total of 5 cases of lower patella fractures treated at our department between February 2020 and September 2021 were identified. The patient group consisted of one male and four females, with an average age of 66 years. All 5 patients underwent fixation using the Suture Bridge technique with 5-Ethibond.
Surgical technique
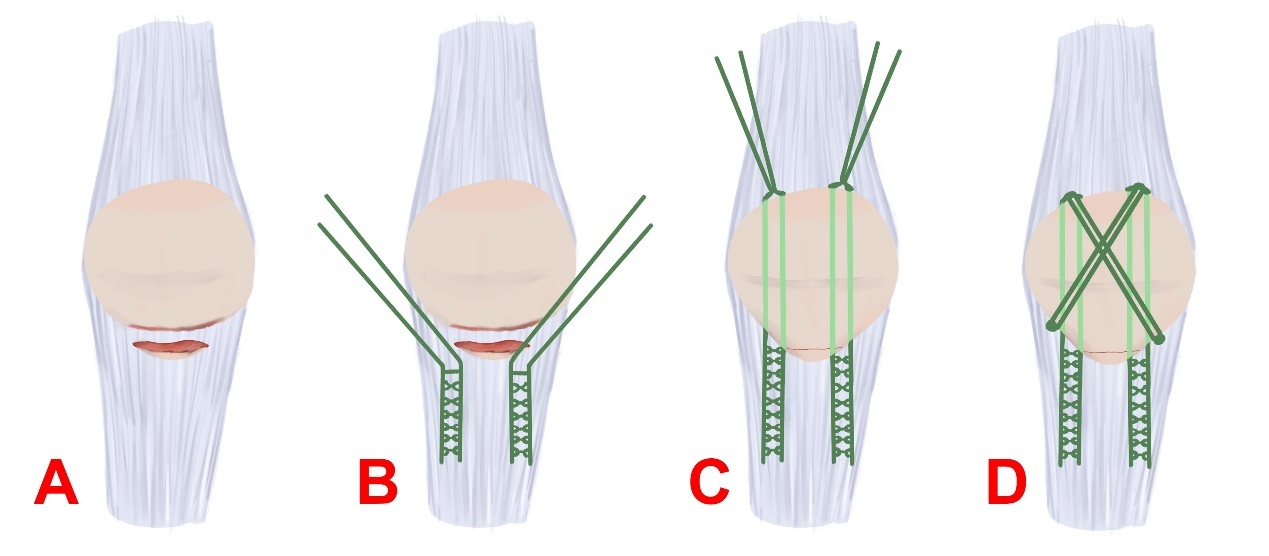
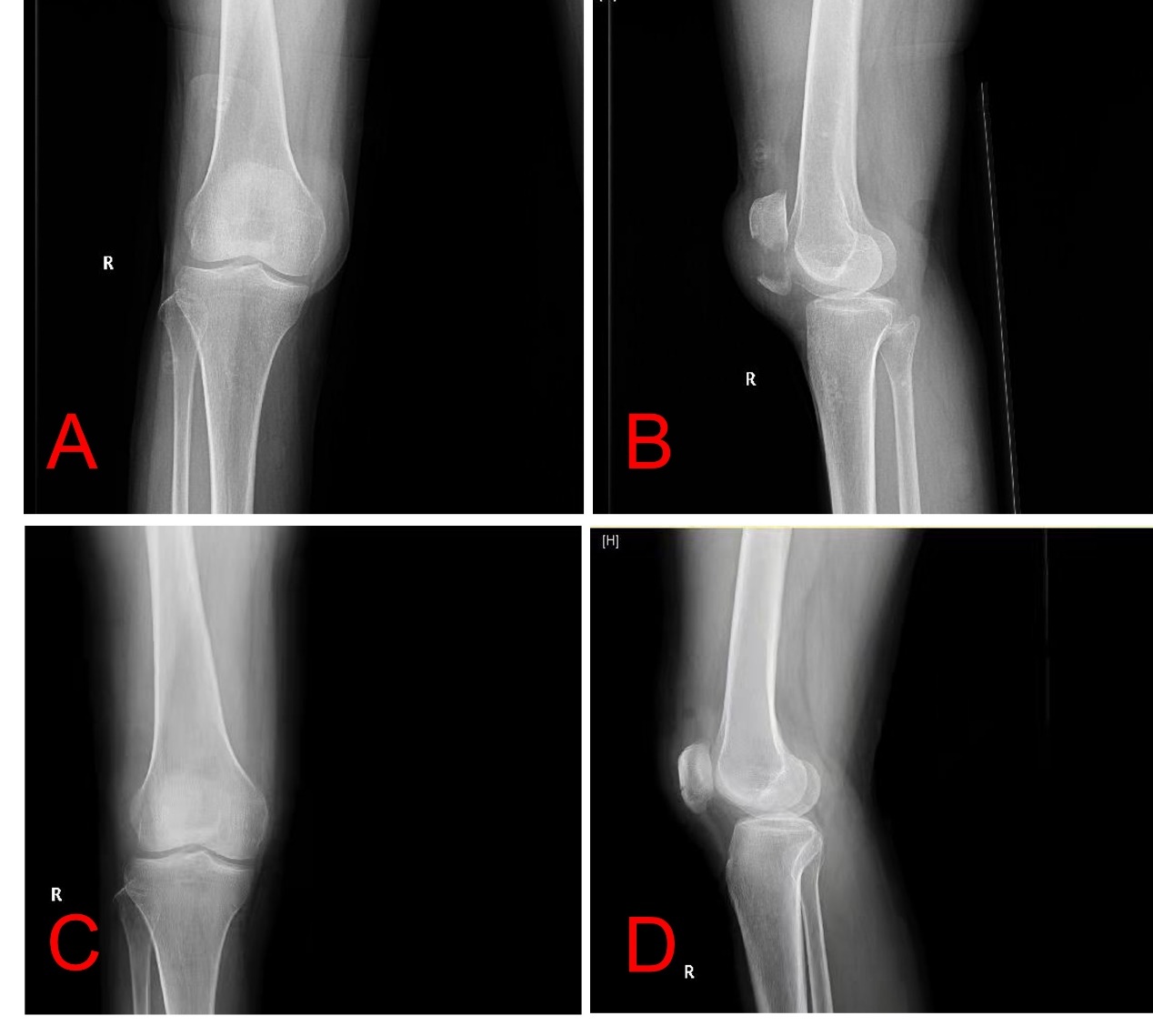
After satisfactory anesthesia, the patient was placed in supine position (Fig. 2A). An anterior median incision was made over the knee, with landmarks based on the patella and tibial tubercle (Fig. 2B). An anterior median is made over the knee to expose the broken end of the fracture. The periosteum was elevated off proximal fracture edges, and fracture hematoma was removed (Fig. 2C).
Next, the knee is placed into extension, and the long axis patella tendon is identified and marked. 5-Ethibond was placed in a Krackow fashion along the medial and lateral edges of the patellar tendon, leaving 4 suture limbs to be passed through the patella (Fig. 2D). Bone reduction forceps are used to assist in the reduction of the fracture, and two Kirschner wires were utilized for temporarily fixation of the patella fracture (Fig. 2E). Vicryl (1#) was used to suture the retinaculum (Fig. 2F).
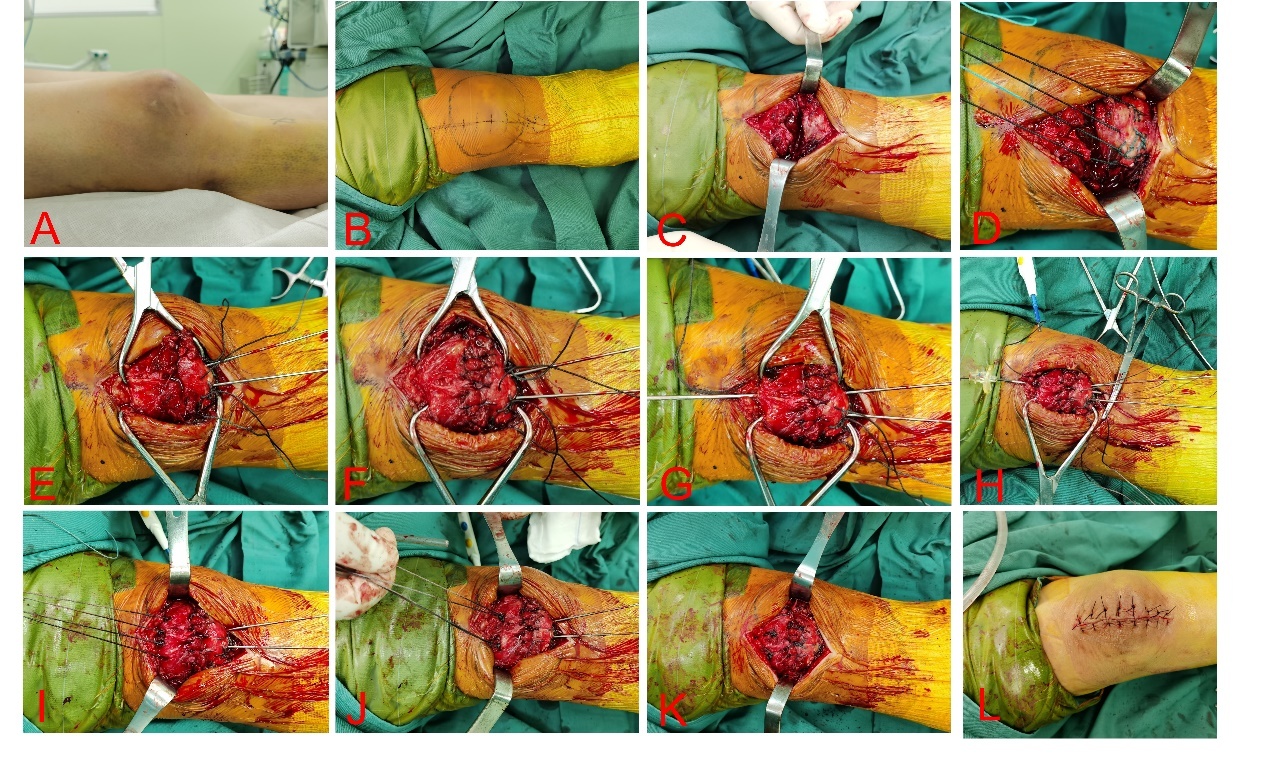
The sutures were passed through the Kirschner wire along the long axis of the patella. Using an electric drill, a 2.0 Kirschner wire was passed through the patella along its long axis (Fig. 2G). After removing the Kirschner wire, a spinal puncture needle was passed through the Kirschner wire tract. A PDS Ⅱ suture was passed through the spinal puncture needle (Fig. 2H). Use PDS II suture to lead the 5-Ethibond tail line out of the patellar tunnel and complete the passage (Fig. 2I). The sutures were then tied at superior pole of the patella with knee in extension (Fig. 2J). The remaining 5-Ethibond tail line is fixed and knotted diagonally below the patella, forming an 8-shaped fixation (Fig. 2K). Reduction is confirmed with fluoroscopy. Then subcutaneous and skin layers were closed in a tension-free manner (Fig. 2L). Final X-rays were obtained confirm the reduction (Fig. 3).
Postoperative care and follow-up
A radiological examination was performed on the day after operation to assess the postoperative condition. The splint external fixation was used for patients as protection postoperatively for 4 weeks. Starting from 2 days after the surgery, patients were encouraged to engage in muscle exercise and weight-bearing activities under the guidance of a rehabilitation therapis. The patients were followed up every 4 to 8 weeks to record range of motion of knee and clinical/radiological fracture healing.
Outcomes Measures
The main outcomes of this study were the reoperation rates, the incidence of soft tissue irritation, fixation failure, infection and knee function.
Results
The mean operation time was 64 minutes, with a range of 50 to 80 minutes. The mean intra-operative blood loss was 51 mL, ranging from 40 to 60 mL. All 5 cases demonstrated well-healed incisions after surgery. The mean follow-up duration was 14.8 months, ranging from 8 to 22 months. All cases showed fracture healing, with an average time of 10.4 weeks (range: 8–12 weeks) after surgery. During the follow-up period, no instances of reduction loss or soft tissue irritation were observed. All patients regained full range of motion within an average of 12.4 weeks (ranging from 10 to 14 weeks) as shown in Table 1. None of the patients complained of anterior knee pain.
Discussion
The fracture of the infrapatellar pole presents a challenge for orthopedic surgeons in achieving stable fixation. To our knowledge, the ideal method for fixing displaced infrapatellar pole fracture has not been identified. Various surgical techniques have been employed, such as tension band wiring, screws, a rim plate, and cannulated screws with tension band wire. However, concerns persist regarding potential issues such as soft tissue irritation, breakage of metal wires, and he development of anterior knee pain.6,7
With the advancement of suture material, suture fixation has emerged as a viable method for treating infrapatellar pole fracture and tendon ruptures.8 Suture fixation has been associated with minimal soft tissue irritation, lower reoperation rate, and favorable knee range of motion and functional.4,9,10
The Suture Bridge technique is a surgical method commonly used in orthopedics for the repair of tendon or ligament injuries, particularly in the shoulder and knee joints. It involves the use of sutures to create a “bridge” between two points of attachment, providing stability, support, and facilitating the healing process. Kim KS et al. reported that in the comminuted inferior pole fractures of the patella, suture bridge anchor fxation resulted in good bony union and satisfactory clinical outcomes during the short-term follow-up.9
Suture anchor fixation involves passing sutures through the bone using specialized anchors. These anchors are carefully inserted into the bone to ensure a secure fixation. The sutures are then tied, securing the fractured fragments or ligaments in place.11,12 5-Ethibond is a type of non-absorbable suture material commonly used in orthopedic procedures. It is known for its strength and durability, making it suitable for applications that require long-term fixation. 5-Ethibond fixation involves using the 5-Ethibond suture to pass directly through the fractured fragments or ligaments, creating a reliable and secure fixation.13,14
It is generally true that the cost of 5-Ethibond suture material is lower compared to the cost of suture anchors. Suture anchor fixation is typically not reversible, as the anchors are securely implanted in the bone. Removal of the anchors may require an additional surgical procedure. 5-Ethibond fixation is reversible as the sutures can be easily removed, allowing for potential revision surgeries or adjustments if needed.
In our study, we explored the use of Suture Bridge technique with 5-Ethibond for fixing infrapatellar pole fractures. At first, we use 2.0mm Kirschner wires to create transosseous tunnels. Then, using 5-Ethibond through the bone tunnel, then tying knots at the upper pole of the patella. It is generally known that transosseous tunnels are considered the “gold standard” for patellar tendon repair. A previous clinical study demonstrated that the effectiveness of suture anchors in addressing extensor mechanism ruptures around the knee surpasses the conventional transosseous tunnel method.15 Another systematic review indicates that in addressing the gap formation in patellar and quadriceps tendon ruptures, the biomechanical attributes of suture anchor fixation may surpass those of traditional transpatellar approaches.16 A biomechanical assessment comparing suture anchor and transosseous tunnel techniques for patellar tendon repair suggests that, in a cadaveric model, suture anchor repair demonstrates comparable biomechanical features to the established transosseous tunnel repair, particularly in cyclic loading and ultimate failure loads. Additionally, a tendency toward reduced gaps is observed in the suture anchor group.17 However, unlike patellar tendon repair, in addition to the transosseous tunnel repair, we ultimately implemented an 8-shaped fixation on the surface of the patella. More importantly, unlike patellar tendon ruptures, in the case of infrapatellar pole fractures, the ultimate healing involves the fusion of bone to bone rather than the healing between tendon and bone. Recently, a study by Zhou, M. et al. indicated that the use of the Krackow suture combined with the suture bridge technique in the treatment of acute inferior patellar fractures can achieve stable fracture fixation with significant clinical utility. In contrast to our study, the Zhou, M. et al surgical procedure is more intricate, especially after drilling four longitudinal tunnels, followed by a horizontal tunnel. This approach may pose a risk of damaging the longitudinal sutures during the transverse drilling process.18 Certainly, the quality of the effect may require more clinical cases for verification.
Our results demonstrated that 5-Ethibond was an effective treatment option for these fractures. Importantly, the use of Suture Bridge technique with 5-Ethibond did not cause irritation to the patellar tendon, and no patient reported discomfort due to the prominence of the implant.
This novel technique also has limitations. At first, we did not conduct a biomechanical test evaluate the stability of the fixation. While intraoperative testing demonstrated a stable fixation, a comprehensive biomechanical evaluation is necessary prior to the widespread clinical application of this technique. Secondly, our study included only five patients who underwent fixation using Suture Bridge technique with 5-Ethibond. The excellent outcomes observed in this small sample may not be fully representative when larger patient cohorts are involved. Given the relatively low incidence of this type of fracture, conducting a multicenter trial would be beneficial to further assess the efficacy and safety of the technique.
In conclusion, our study provides promising results regarding the use of Suture Bridge technique with 5-Ethibond for treating infrapatellar pole fractures. However, further research involving biomechanical testing and larger-scale clinical trials is warranted to validate the findings and establish the technique’s broader applicability and long-term outcomes.
Ethics approval and consent to participate
The study was approved by the ethics committee for clinical research at Northern Jiangsu People’s Hospital. Written informed consent was obtained from all patients prior to commencement of the study.
Availability of supporting data
All data are fully available without restriction.
Conflict of interest
The authors declare that they have no competing interests.
Funding
None.
Authors’ contributions
Liang Y and Chen PT conceived of the design of the study. Hu JL, Zhang P, Liang Y, Zhang JL, Wang JC participated the experiment. He JS analyzed the data. Liang Y and Hu JL finished the manuscript. All authors read and approved the final manuscript.
Acknowledgments
Not applicable.