Introduction
Intertrochanteric femur fractures (IFF) are extra-articular fractures and represent a common injury among the elderly population, with approximately 90% occurring in patients over 65 years of age. These fractures account for nearly 50% of all proximal femur fractures and are associated with a high mortality rate, ranging from 4.5% to 22%. Additionally, they result in significant functional impairment.1
The management of IFF is challenging due to the complexity of the fracture pattern and the difficulty in achieving anatomical reduction and stable fixation. As life expectancy continues to increase, the incidence of IFF is expected to rise. In the United States, for instance, there were 250,000 cases of IFF reported in 2004, with 90% of these occurring in individuals aged 70 and older. The post-fracture mortality rate ranges from 15% to 20%, and the annual healthcare costs for treating these fractures amount to approximately $10 billion.2 It is projected that by 2040, there will be around 500,000 cases of proximal femur fractures worldwide each year.2
In Vietnam, according to data from the Hospital for Traumatology and Orthopaedics, there are nearly 700 cases of IFF that require treatment each year. The conventional treatment options for unstable IFF include the use of proximal femoral nails (PFNAs) and Trigen InterTan (IT) nails. PFNA and IT are often preferred due to their biomechanical advantages and low failure rates, resulting in favorable clinical outcomes. The IT nail, designed with two screws in the femoral neck region and an integrated compression mechanism, allows for axial compression and rotational stability of the femoral neck fragment.3
Recently, minimally invasive techniques, including intramedullary nailing, fluoroscopy, and the use of a fracture table, have been employed at the Hospital for Traumatology and Orthopaedics based on insights gained from international literature and practical experience. To contribute to the evaluation of treatment effectiveness and to inform appropriate treatment choices for IFF, our research team conducted an assessment of the outcomes of IFF treatment using the Trigen InterTan nail at the Hospital for Traumatology and Orthopaedics.
Objective: The objective of this study is to evaluate the outcomes of IFF treatment using the Trigen InterTan (IT) nail at the Hospital for Traumatology and Orthopaedics.
Material and Methods
Study Population
A total of 35 patients diagnosed with intertrochanteric fractures treated using the Trigen InterTan nail at the Lower limb department, Emergency Department, Hospital for Traumatology and Orthopaedics during the study period (02/2021-08/2021) were included in the research. Ethics approval was granted at Pham Ngoc Thach University of Medicine.
Sample Selection Criteria
Patients aged 18 and above.
Fractures located in the intertrochanteric region resulting from trauma.
Patients who underwent surgery with bone fixation using the Trigen InterTan nail at he Lower limb department, Emergency Department, Hospital for Traumatology and Orthopaedics.
Patients who provided informed consent to participate in the study.
Exclusion Criteria
Patients who did not consent to participate in the study.
Patients with pre-existing fractures in the upper part of the femur.
Intertrochanteric fractures due to pathological causes.
Intertrochanteric fractures in patients with advancing infections.
Patients with pre-existing paralysis or inability to ambulate before the intertrochanteric fracture occurred.
Patients with medical conditions or overall health status that precluded surgery (ASA grade 5).
Study Design
This study followed a retrospective, descriptive case series design.
Data Analysis
The study results were coded and analyzed using Stata 14.0 software. The findings were presented in the research report using tables, charts, and figures created with Word 2019.
Results
From February 2021 to August 2021, we conducted a study on 35 patients diagnosed with intertrochanteric femur fractures treated with Trigen InterTan nails at the Department of Orthopedics and Emergency, Ho Chi Minh City Orthopedic and Trauma Hospital.
Patient Characteristics
The average age of patients in our study was 70.97 ± 16.97 years, with the youngest being 19 years old and the oldest 97 years old.
In our study sample, the male-to-female ratio was 2.89:1 (74.29% female, 25.71% male).
The most common cause of intertrochanteric fractures was self-falls (77.14%), followed by motor vehicle accidents (17.14%), and occupational accidents (5.71%).
Nearly 74.29% of patients had internal medical comorbidities, with 34.3% having one internal medical condition and 39.99% having two or more.
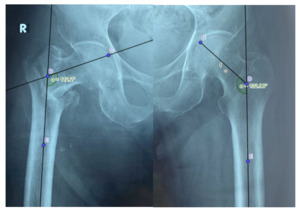
According to the AO classification, type A2 fractures were the most common (57.14%), followed by A1 and A3 fractures at 20% and 22.86%, respectively.
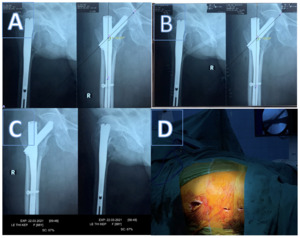
Surgical Outcomes
At the final assessment, 97.14% of cases achieved bone union, with only 1 case (2.86%) showing non-union.
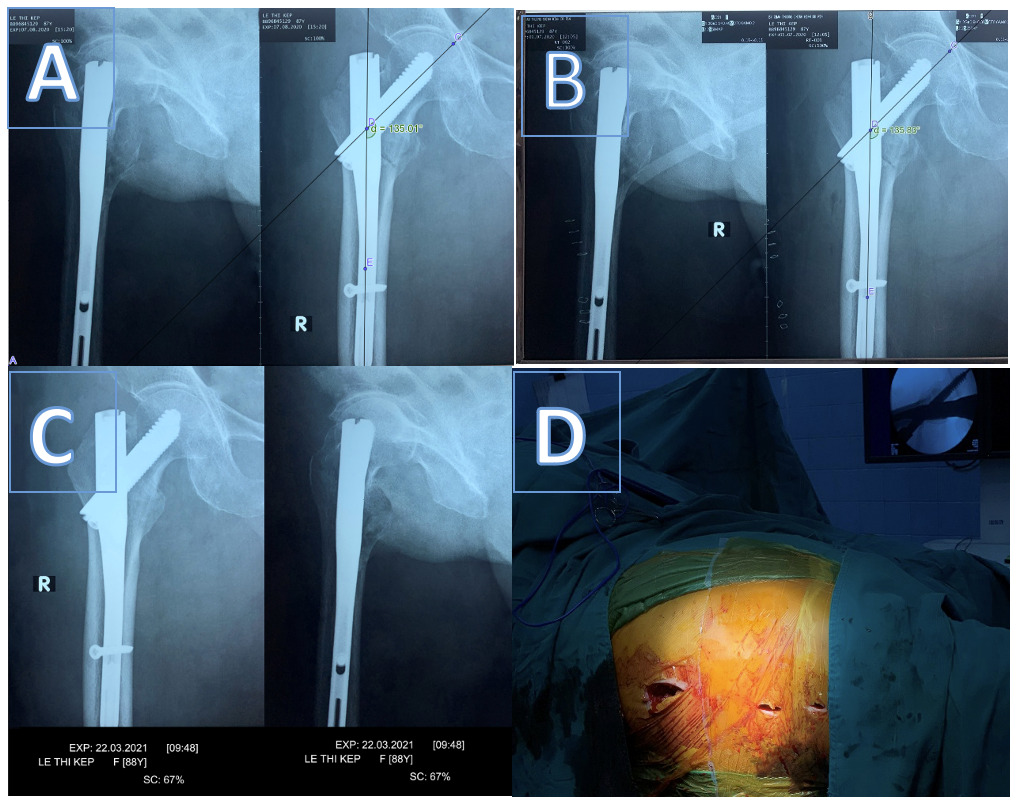
Six months post-surgery, 27 cases had no shortening (77.14%), 7 cases had shortening < 1.5 cm compared to the unaffected side (20%), and 1 case had shortening between 1.5 – 2.5 cm (2.86%).
Recovery of neck-shaft angle immediately post-surgery compared to the unaffected side: 9 cases had their neck-shaft angle restored to that of the unaffected side (25.7%), 5 cases had a larger neck-shaft angle post-surgery (14.3%), and 21 cases had a smaller neck-shaft angle post-surgery, ranging from 1 to 15 degrees smaller than the unaffected side (40%).
Change in neck-shaft angle at the final assessment compared to immediately post-surgery: nearly 70% of cases showed no change in the neck-shaft angle of the femur six months after surgery, while 30% exhibited a decrease (varus deformity), with the majority experiencing a decrease of 1 – 5 degrees (22.86%).
Functional Recovery
At the final assessment, over 27 cases had no pain in the hip region (77.14%), 5 cases reported mild pain (14.29%), 2 cases experienced moderate pain (5.7%), and 1 case had severe pain (2.86%).
After 6 months, the majority of cases were able to flex their hips > 90 degrees (94.29%).
Based on the Harris Hip Score at six months, the average score was 81.94 ± 12.12 points. Among these cases, 65.7% exhibited very good hip joint function, and the rest demonstrated good function.
Complications of the Treatment Method
The mean surgical duration was 60 minutes, with the shortest surgery lasting 30 minutes and the longest 130 minutes.
The average intraoperative blood loss was 160.86 ± 72.8 ml, with the least being 50 ml and the most being 300 ml.
In 57.14% of cases, blood transfusions were performed during surgery, with an average transfusion volume of 203.43 ± 189.29 ml and a range of 230 ml to 500 ml.
At the final assessment, we recorded 33 cases with no early complications (94.29%) and 2 cases with early complications (5.72%), including one case of postoperative pneumonia (2.86%) and one case of superficial wound infection (2.86%). (Table 1)
We did not observe any cases of surgical site bleeding, venous thrombosis, or pressure ulcers. All patients in the study were discharged safely.
In terms of late complications, 31 cases had no complications (88.57%), 2 cases had malunion (5.72%), 1 case had osteomyelitis (2.86%), and 1 case had deep late infection (2.86%). (Table 2)
Discussion
Our study involved an investigation of 35 patients with an average age of 70.97 ± 16.97 years, ranging from 19 to 97 years old. A substantial proportion of patients, 21 out of 35 (60%), were over 70 years old. The results of our study align with several domestic and international studies, including works by authors such as Nguyen Van Tien Luu, Nguyen Anh Tuan, Duong Thanh Binh, Appelt, Aktselis, and Zhang.3–8
In our study, females accounted for 74.3% of the participants, resulting in a female-to-male ratio of 2.89:1. This finding is consistent with previous research conducted both domestically and internationally, including studies by Nguyen Anh Tuan, Duong Thanh Binh, Aktselis, and Zhang.3,4,6,7
The most common cause of proximal femoral fractures in our study was falling directly onto the buttocks, accounting for 27 patients (77.14%). The second most common cause was traffic accidents, involving 6 patients (17.14%), followed by occupational accidents with 2 patients (5.71%). Our results are in accordance with those of other authors, including Nguyen Van Tien Luu, Le Quang Tri, Duong Thanh Binh, and Radaideh.3,8–10
Within our study sample, 26 cases (74.29%) had at least one accompanying internal medical condition. Among them, 34.3% of patients had one internal medical condition, and 40% had two or more internal medical conditions. Our findings are consistent with numerous studies conducted both domestically and internationally, such as those by Nguyen Van Tien Luu, Le Quang Tri, Duong Thanh Binh, and Palm.3,8,9,11
Our study revealed that type A2 fractures were the most common, accounting for 57%, while type A1 and A3 fractures were less frequent, with nearly equal proportions of 20% and 23%, respectively. These results are consistent with findings from studies conducted by Nguyen Van Tien Luu, Nguyen Anh Tuan, and Radaideh.7,8,10 In elderly individuals, intertrochanteric fractures typically result from falls, often with an indirect impact on the hip. Although the traumatic force is not substantial, the majority of these fractures are comminuted and complex due to the patients’ osteoporotic conditions. Our study also observed that type A2 fractures were more common in females (45.7%), whereas reverse type A3 fractures were more common in cases involving high-energy trauma mechanisms. In contrast, type A1 and A2 fractures occurred more frequently in cases involving mild trauma. This difference was statistically significant with a p-value of 0.01.
We observed that 97% of patients achieved fracture union. This rate is consistent with findings from other studies conducted by Nguyen Van Tien Luu, Nguyen Anh Tuan, Duong Thanh Binh, Wu, and Zhang.3,6–8,12 This high union rate can be attributed to the primarily cancellous bone structure and rich blood supply in the proximal femur, which favor the union process.
The percentage of shortening in our sample was 22.86%, with 20% experiencing less than 1.5 cm of shortening, and only one case (2.86%) with shortening ranging from 1.5 to 2.5 cm. There were no cases with shortening exceeding 2.5 cm. These results closely align with findings from studies by Nguyen Van Tien Luu, Nguyen Huy Thanh, Duong Thanh Binh, and Singh.3,8,13,14
Approximately 57.14% of patients received blood transfusions during surgery, with an average transfusion volume of 203.43 ± 189.29 ml. This outcome is consistent with several other studies, including those by Phi Manh Cong, Nguyen Anh Tuan, Wu, Zhang, and Singh.6,7,12,13,15
We observed that 33 cases (94.29%) did not experience early complications, while 2 cases (5.72%) developed early complications, including one case of postoperative pneumonia (2.86%) and one case of superficial surgical site infection (2.86%). No cases of surgical site bleeding, venous thrombosis, or pressure ulcers were recorded. All patients in the study were discharged safely. Our findings indicate that the combination of intramedullary nail fixation and minimally invasive surgery is relatively safe. The rate of early complications in our study was quite low, consistent with previous publications by Phi Manh Cong, Nguyen Van Tien Luu, Dankai Wu, Zhong, and Singh.8,12,13,15,16 This suggests that intramedullary nail fixation with Triger Intertan is a relatively safe surgical approach for proximal femoral fractures, especially in elderly patients with comorbidities.
In our study, there were no cases of device failure, refracture, or cut-out. We observed a late complication rate of 11.43%, which included one case of delayed deep infection (2.86%) and two cases of varus collapse (5.7%).
No patients in our study died from the time of proximal femoral fracture until the 6-month postoperative period. This may be attributed to the limited number of patients aged 80 or older in our study, with a mean ASA score of 2.17 ± 0.51, and only 20% of the study population having an ASA score of 3 or higher. Additionally, our study had a relatively small sample size and short follow-up duration, which may not accurately reflect the mortality rate associated with proximal femoral fractures.
Conclusion
In conclusion, our study provides valuable insights into the demographics, fracture patterns, mechanisms of injury, comorbidities, surgical outcomes, and complications of ntertrochanteric femur fractures. The results of our study are consistent with existing literature and suggest that treating intertrochanteric femur fractures with IT nail is a safe and effective approach for treating these fractures, especially in elderly individuals with comorbidities.
Corresponding Author
Phi Duong Nguyen
https://orcid.org/0000-0002-9556-4049
Institution: City Children’s Hospital
Address: 15 Vo Tran Chi Street, Tan Kien ward, Binh Chanh District, Ho Chi Minh City, Vietnam
Email: nguyenduongphi1311@gmail.com