Introduction
Bone is a common site of metastasis in patients with solid tumors with a cumulative incidence of 8.4% at 10 years, and approximately 400,000 new cases of malignant bone metastasis are diagnosed in the United States each year.1,2 Metastatic bone disease (MBD) is especially common in patients with advanced prostate, breast, renal, and thyroid cancer as well as multiple myeloma.1,2 The most common location for metastasis in the appendicular skeleton is the proximal femur with one-third of metastatic lesions to bone occur occurring in this location. Due to the mechanical forces transmitted through the proximal femur during weightbearing, these lesions often present with functional pain and disability, and up to 29% of patients with proximal femur MBD develop pathologic fractures.2–4
The goals of surgical treatment of MBD about the hip are fracture stabilization, pain reduction, and restoration of function. The durability of the construct should exceed the projected life expectancy of the patient and should allow for immediate weightbearing if possible. Treatment options for impending and complete pathologic fractures of the proximal femur due to MBD include intramedullary nails (IMN), open reduction and internal fixation (ORIF) with plate and screw constructs, and resection with arthroplasty reconstruction.5,6 The poor healing potential and higher rate of nonunion seen in metastatic lesions and pathologic fractures can lead to hardware failure with ORIF or IMN, especially in patients with longer life expectancy, and increased length of survival has been shown to be an independent predictor of hardware failure.7,8 With advances in medical management for metastatic disease, particularly in patients with prostate and breast cancer, implant durability has become even more important as patient life expectancy increases.
In patients with metastatic lesions of the femoral head and neck, with or without acetabular involvement, resection and arthroplasty is the preferred treatment.5,9 Isolated metastatic lesions of the proximal femur can be treated with hemiarthroplasty or total hip arthroplasty (THA). THA is used if acetabular lesions are present, and proximal femur replacement (PFR) is the treatment of choice if there is extensive pertrochanteric bone loss.10,11 Arthroplasty provides a durable reconstruction that allows for immediate weightbearing in patients with proximal femur MBD with equivalent functional outcomes to patients treated with IMN. Studies have shown that PFR has improved implant survival when compared to IMN or ORIF, and the literature supports resection with endoprosthetic reconstruction in patients with good overall prognosis and prolonged life expectancy.12
While there is a large body of literature examining hip arthroplasty in osteoarthritis and non-pathologic femoral neck fractures,13 data on arthroplasty outcomes in patients with proximal femur MBD is limited.14–16 The purpose of this investigation was to examine the rates of reoperation and other complications, as well as postoperative functional outcomes, in patients undergoing primary hip arthroplasty for MBD.
Methods
Ethical Considerations
As this was a retrospective records review, the project was determined to be exempt from review by our center’s Institutional Review Board within the Human Subjects Protection Division (project number 21112902-IRB01). Patient data were de-identified and compliant with the Health Insurance Portability and Accountability Act.
This was a retrospective review of patients with hip MBD who underwent primary hip arthroplasty at a single institution between 2007 and 2021. The study was approved by our center’s Institutional Review Board. Patients who received hemiarthroplasty, total hip arthroplasty, and proximal femur replacement were included. PFR and THA that involved complex acetabular reconstruction were combined into a complex arthroplasty group. Patients who underwent hip arthroplasty as a revision procedure after prior arthroplasty or internal fixation for MBD were excluded. Indications for arthroplasty were impending or complete pathologic fracture, resection and reconstruction for oligometastatic disease, and advanced osteoarthritis in patients with concurrent MBD of the hip. All patients who survived the perioperative period had a minimum follow-up of six months. Median follow-up for surviving patients was 2 [1-4] years. Demographics, histopathologic diagnosis, surgical details, and outcomes including rates of reoperation and survival were collected. The primary outcome was reoperation. Secondary outcomes were surgical complications, periprosthetic joint infection, periprosthetic fracture, overall survival, and postoperative function. Preoperative and postoperative ambulatory function were classified as bedridden, wheelchair-bound, ambulatory with an assistive device, or ambulatory without an assistive device. Preoperative ambulatory function was determined based on function at the preoperative visit closest to surgery and prior to fracture in those patients who presented with pathologic fracture. Postoperative ambulatory function was determined at final follow up.
Statistical analysis
Descriptive statistics were used to report patient demographic and clinical characteristics as well as outcome measures. Continuous variables were described as medians with interquartile range (IQR) or means with standard deviation (SD) depending on normality. McNemar’s test was used to compare preoperative and postoperative ambulatory function. Kaplan-Meier analysis was used to determine overall survival. P<0.05 was considered significant.
Results
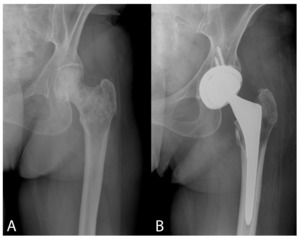
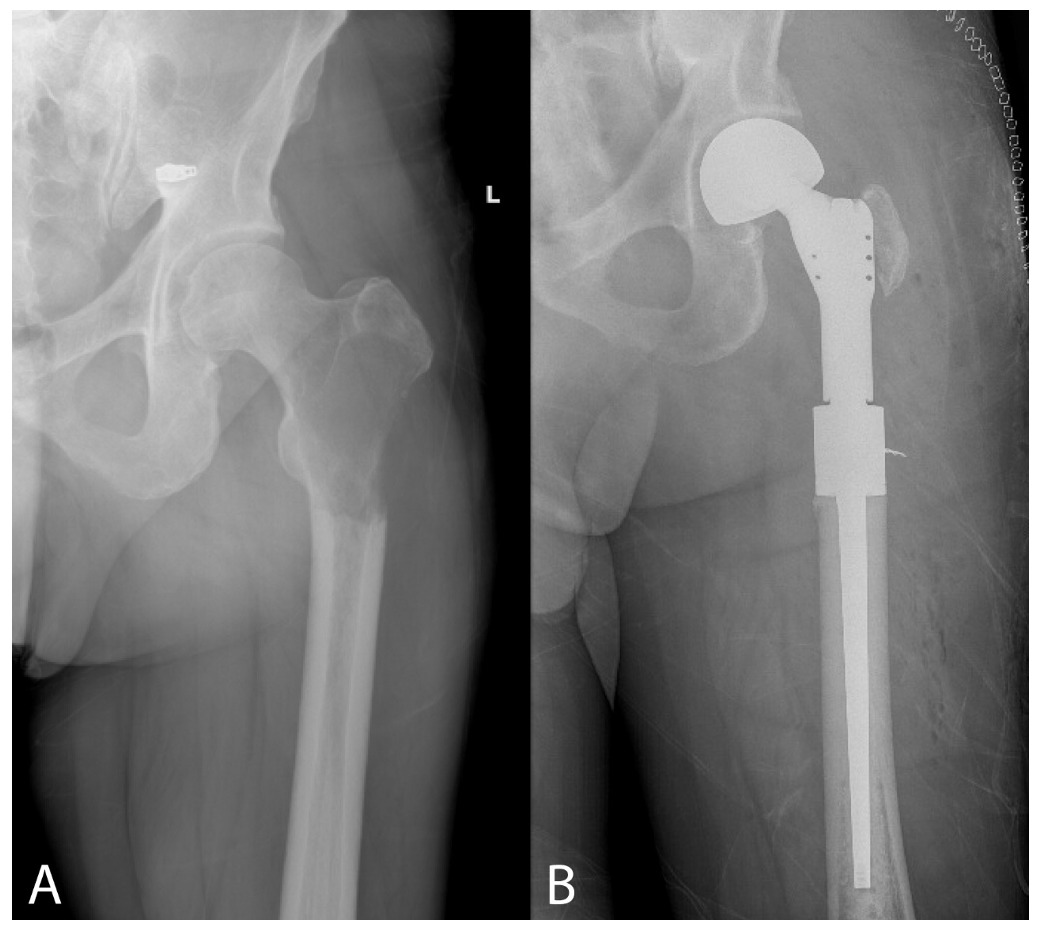
Ninety-three cases in 91 patients were included in the study with two patients undergoing bilateral procedures. Demographics and clinical characteristics of this patient population are detailed in Table 1. This cohort consisted of 52 (57.1%) women and 39 (42.9%) men with a median age of 62 [54.0-71.3] years. The most common histopathologic diagnosis was metastatic breast cancer (31.9%), followed by metastatic lung, renal, and prostate cancer. Five (5.5%) patients had metastatic sarcoma and 4 (4.4%) had multiple myeloma. Hip arthroplasty was performed for pathologic fracture in 44 (47.3%) cases and for impending pathologic fracture in 34 (36.6%) cases. In the remaining cases, the indication for arthroplasty was pain related to advanced osteoarthritis in hips with concurrent MBD (n=12) or for resection of oligometastatic disease (n=3). THA was performed in 52 cases (55.9%) (Figure 1), hemiarthroplasty was performed in 15 (16.1%), and complex arthroplasty was performed in 26 (28%) (Figure 2). Median operative time was 107 [82-135] minutes. Following the procedure, 31 (34.1%) patients underwent adjuvant radiotherapy to the operative hip.
Median survival was 10.4 [3.7-23.7] months. Overall survival was 60.2% at six months, 53.3% at one year, 27.6% at three years, and 13.5% at five years postoperatively (Figure 3). Three patients died during hospital admission. Two had unrelated complications secondary to their metastatic disease burden during hospitalization and were transitioned to comfort care before expiring. One patient who underwent a cemented hemiarthroplasty had an episode of hypotension intraoperatively. He was resuscitated but was unable to be weaned off pressor support and died on postoperative day 3.
Eleven (12.1%) patients sustained at least one complication, and three (3.3%) patients sustained multiple complications. Complications included superficial wound infection (n=1), hematoma (n=2), periprosthetic joint infection (n=2), dislocation (n=6), periprosthetic femur fracture (n=2), acetabular component loosening (n=4), and femoral component loosening (n=1). There were two periprosthetic joint infections. One patient was treated with chronic suppressive antibiotics due to her poor prognosis, and the other patient underwent irrigation and debridement with partial component exchange followed by a Girdlestone resection arthroplasty for recurrent infection. Postoperative dislocations occurred in six cases, two in hips treated with primary THA and four in hips treated with complex arthroplasty.
Complications lead to 11 reoperations in five (5.5%) patients. Implant survival is shown in Figure 4, with 92.9% survival at 1 year and 89.8% survival at 5 years after the index procedure. All patients who underwent reoperation had THA (n=4) or complex arthroplasty (n=1) as their initial procedure. No dislocations or reoperations occurred in patients treated with hemiarthroplasty. One patient sustained a periprosthetic femur fracture and underwent revision to a proximal femur replacement. A second patient noted increasing groin pain 18 months after THA and radiographs demonstrated aseptic loosening of the acetabular component. This patient had a history of pelvic radiation and poor acetabular bone stock with protrusio acetabuli noted at his initial surgery. He underwent acetabular component revision with a tantalum trabecular metal cup and augment. The third patient sustained a dislocation after complex arthroplasty with imaging showing aseptic loosening of the acetabular component with bone loss. She underwent a Girdlestone procedure due to poor acetabular bone and to enable continuation of systemic therapy for metastatic disease.
Two patients underwent multiple reoperations. One patient with a history of radiation to the hip and pelvis endorsed increasing hip and groin pain 10 months after THA, and imaging demonstrated aseptic loosening of the acetabular component. She underwent revision to a tantalum trabecular metal cup. Three years later, she had the acute onset of hip pain and was found to have a prosthetic hip dislocation which necessitated open reduction and conversion to a modular dual mobility liner, followed by a recurrent dislocation and revision to a constrained liner. The final patient also had a history of hip and pelvis radiation and sustained a periprosthetic fracture one year after THA with evidence of femoral component loosening. He underwent revision of the femoral component complicated by persistent drainage from his surgical wound necessitating irrigation and debridement. Eighteen months after his initial THA, he sustained a prosthetic dislocation and radiographs demonstrated loosening of the acetabular component. He underwent revision of the acetabular component with a tantalum trabecular metal cup. He subsequently re-dislocated and had recurrence of his periprosthetic joint infection. He elected to undergo irrigation and debridement with revision of the femoral component to increase offset and stability. During his postoperative recovery, he sustained another dislocation and underwent a Girdlestone procedure for recurrent instability and infection.
Preoperatively, 16 (17.6%) patients were able to ambulate independently, 45 (49.5%) were able to ambulate with an assistive device, 17 (18.7%) were wheelchair-bound, and 13 (14.3%) were bedridden. At final follow up, 32 (35.2%) patients could ambulate independently, 53 (58.2%) could ambulate with an assistive device, and 3 (3.3%) patients were wheelchair-bound. No patients were bedridden postoperatively, and 3 (3.3%) patients died during admission and did not have postoperative function at follow up. In the 88 patients who survived to discharge, 85 (96.6%) were able to ambulate independently or with an assistive device after surgery. Overall, ambulatory functional status was improved in 48.4% of patients, maintained in 44.0%, worsened in 4.4%, and not recorded in the 3.3% of patients who died during admission. There was a significant increase in the proportion of patients who were able to ambulate independently (35.2% vs 17.6%; p=0.02) and a significant decrease in the number of patients confined to a wheelchair (18.7% vs 3.3%; p=0.045) after surgery.
Discussion
The proximal femur is a frequent location for metastatic lesions which can lead to significant pain and functional limitations. These lesions are at high risk for pathologic fracture, and 65% of all pathologic fractures that require surgery occur in the proximal femur.2,17 The goals of treatment of MBD about the hip are to relive pain, restore function, improve quality of life, and facilitate custodial care and treatment of the primary disease. Studies have explored various treatments for proximal femur MBD, including IMN, ORIF, and resection with reconstruction using standard arthroplasty components or proximal femur replacement. These investigations support arthroplasty as the treatment of choice for metastatic lesions of the femoral head and neck and PFR for lesions causing extensive subtrochanteric bone loss.5,6,9,18 These interventions are associated with reduced rates of complications and implant failure when compared to ORIF and IMN, especially in patients with prolonged life expectancy.7,8,19 However, many studies examining treatment of MBD of the hip report only short-term outcomes or results of treatment with PFR alone or compared to fixation.14–16 There is a relative paucity of data on longer-term outcomes and complications in patients with MBD of the hip treated with primary arthroplasty that includes hemiarthroplasty, THA, and PFR.
Overall survival in patients who have received surgical treatment for MBD of the proximal femur is poor. Houdek et al. reported survival of 42%14 and Selek et al. reported survival of 27%20 of patients one year after treatment of proximal femur MBD with endoprosthetic reconstruction. Hayden et al. noted a one-year survival rate of 38% after treatment of hip MBD with THA or hemiarthroplasty.15 In our cohort, the median survival was 10.4 months and 53.3% of patients survived to one year postoperatively. This is consistent with these and other previous studies reporting rates of one-year survival ranging from 17% to 69% and median survival less than one year following surgical treatment of proximal femur metastatic disease.21,22 Although mortality rates in patients with metastatic cancer remain high, improved cancer screening and early diagnosis combined with advances in medical treatments have improved survival in patients with metastatic breast, prostate, and lung cancer among others.23 These patients may now live long enough to experience implant failure, and studies have shown that increased postoperative survival is an independent predictor of implant failure in pathologic long bone fractures.8 Given the increasing life expectancy of patients with metastatic cancer, treatment of MBD of the hip with durable implants that outlive patients with minimal complications is of utmost importance.
Patients with active malignancy have been shown to have increased rates of postoperative complications after hip arthroplasty.24 In our cohort, 12.1% of patients had postoperative complications, which is consistent with previous studies examining reconstruction with endoprostheses and standard arthroplasty in MDB of the hip.14,20,22 An especially concerning complication after arthroplasty in patients with metastatic disease is periprosthetic joint infection.25,26 Increased infection rates in patients with malignancy is the result of immunodeficiency and wound healing problems caused by chemotherapy and radiotherapy, larger surgical wounds with more extensive resection, and longer duration of surgery among other factors.27 Jakofsky et al. reported a 10% rate of periprosthetic joint infection after arthroplasty for MBD and a rate of 21% in patients with preoperative radiotherapy.4 Additional studies note infection rates of 5-15% in patients who have undergone tumor resection and endoprosthesis reconstruction with risk factors for infection including radiotherapy, revision surgery, and poor soft tissue condition.28 In our study, two patients sustained periprosthetic joint infections, and both patients had a history of preoperative radiotherapy to the operative hip and pelvis. Given the increased risk of wound healing and infectious complications associated with preoperative radiotherapy, some authors advocate for early surgical intervention for MBD of the hip instead of conservative treatment with initial radiotherapy,29,30 though this is not always possible. Another major complication associated with hip arthroplasty for MBD is dislocation.31 THA has a known higher risk of dislocation than hemiarthroplasty both in patients operated on for MBD and for non-pathologic femoral neck fractures.32 A study by Wedin and Bauer of patients treated for proximal femur MBD demonstrated a rate of dislocation that was five times greater in patients treated with THA than in those treated with hemiarthroplasty.6 Additionally, the risk of dislocation in PFR is high due to extended surgical exposure, extensive bone and soft tissue resection, and difficulty with abductor healing to the implant, with rates of dislocation ranging from 2-22% in the literature.33,34 We observed a dislocation rate of 6.5% in our patient population, which is similar to prior studies. All dislocations occurred in patients treated with THA or complex arthroplasty, which included THA with complex acetabular reconstruction and PFR using femoral and acetabular components. There were no dislocations in hips treated with hemiarthroplasty. There is currently a lack of consensus among orthopedic oncologists regarding the use of hemiarthroplasty versus THA in treatment of MBD of the femoral head and neck in patients with good prognoses.35 Physicians must weigh the risks of increased dislocations, operative time, and blood loss with THA against the risk of acetabular wear with hemiarthroplasty necessitating conversion to THA in patients with a longer life expectancy.10
Complications led to reoperation in 5.5% of patients in our cohort, similar to previous reports in patients treated for hip MBD.15,34,36 Hayden et al. reported an overall reoperation rate of 5.3% in patients treated with hemiarthroplasty or THA for pathologic femoral neck fracture,15 and Janssen et al. reported an 11% rate of reoperation in patients with proximal femur MBD treated with PFR.36 However, in our study, 88 out of 93 hips (94.6%) did not require reoperation, and the implant outlived the patient. Four out of five patients who required reoperation had THA as their initial procedure, though this may reflect the high rate of THA procedures done in our patient population. The most common indications for reoperation in our patients were dislocation and acetabular component loosening. Four patients in our study underwent acetabular revision for aseptic loosening, and three of these patients had a history of radiotherapy to the operative hip or to the pelvis. Radiation-induced bone changes negatively affect osseointegration and have been reported to lead to implant failure with rates of aseptic acetabular component loosening as high as 44-52% in both early-generation cemented and non-cemented implants.29,37 Highly porous tantalum trabecular metal acetabular components have been shown to be a promising option for THA in patients with a history of hip and pelvic radiation.38,39 A study by Joglekar et al. examined outcomes of 22 hips undergoing primary THA using tantalum trabecular metal cups in patients with genitourinary, colon, and hematologic malignancies who had previously undergone pelvic radiotherapy. At 5-year follow-up, there were no revisions for acetabular component loosening. The authors attributed this to the high coefficient of friction and bony ingrowth potential of tantalum trabecular metal, as well as the use of multiple multi-angled screw fixation and cementing the liner into the cup to create a unified construct that provides maximal initial fixation and prevents motion during the early postoperative period.39 All three patients in our cohort with a history of pelvic radiation who had loosening of their acetabular components underwent revision with tantalum trabecular metal acetabular cups. None of these patients subsequently needed additional revision surgery for acetabular component loosening. In patients with hip MBD and a history of radiotherapy to the hip or pelvis, consideration should be given to the use of tantalum trabecular metal acetabular components for acetabular reconstruction, especially in patients with advanced acetabular bone loss and poor bone quality.
Many patients who present with proximal femoral metastatic lesions have severe pain with ambulation or are unable to walk. In our patient population, 33% of patients were bedridden or confined to a wheelchair preoperatively, and only 17.6% were able to ambulate independently. Treatment with primary arthroplasty led to restoration of functional ambulation in the majority of patients. No patients were bedridden after surgery, and greater than 95% of patients who survived to hospital discharge were able to ambulate with or without an assistive device. Overall, ambulatory function was improved or maintained in 92.4% of patients, which is one of the core goals of surgery for MBD.
Primary hip arthroplasty may also be considered as a palliative procedure in patients who are severely limited by hip osteoarthritis in the setting of concurrent MBD. Degenerative changes in the native hip may be accelerated by radiotherapy, and patients with malignancy have increased risk of avascular necrosis of the femoral head due to chemotherapy and the hypercoagulable state associated with cancer.40 Surgeons may be reluctant to perform arthroplasty in patients with metastatic disease due to the higher risk of complications in these patients and the perceived high risk to benefit ratio in patients with short life expectancy. Literature on hip arthroplasty in this setting is limited, but case reports demonstrate that elective hip arthroplasty for disabling hip osteoarthritis in patients with advanced cancer allows for pain relief and improved function that leads to enhanced quality of life.40 In our study, 12 patients underwent primary hip arthroplasty for pain and disability related to advanced osteoarthritis with concomitant MBD about the hip but without complete or impending pathologic fracture. After surgery, more than half of these patients (58.3%) had improvement in their ambulatory function and the remainder maintained their level of preoperative ambulatory function. As patients with metastatic disease live longer, increased concurrence of MBD and advanced osteoarthritis should be expected. Elective hip arthroplasty in the setting of symptomatic hip arthritis in patients with MBD should be considered as a palliative procedure that can provide relief from pain and enable patients to live as actively as possible until death.
Limitations
This study has several limitations. It was a single center, retrospective study and subject to the biases inherent in retrospective analysis. The choice of reconstruction technique was at the discretion of the treating surgeon and based on individual patient factors rather than randomization or institutional protocols. At our high-volume arthroplasty center, surgeons may have been more likely to treat with THA, as evidenced by other similar series that report higher percentages of patients treated with hemiarthroplasty.15 Additionally, our goal was to assess outcomes and complications in this group of patients with hip MBD who received primary arthroplasty as a whole. As such, we did not perform detailed comparisons between hemiarthroplasty, THA, and PFR, though we noted fewer dislocations and reoperations in patients with hemiarthroplasty. Finally, validated patient reported outcomes such as the Musculoskeletal Tumor Society rating or the Harris Hip Score were not available in a sufficient number of patients to enable analysis. However, assessment of ambulatory status pre- and postoperatively was used to help assess functional outcome, similar to previous studies in this patient population.41
Conclusions
As advances in cancer care allow patients with metastatic bone disease to live longer, patients with hip MBD require a reconstructive option that will exceed their lifespan. Primary hip arthroplasty provides the majority of MBD patients with a durable reconstruction that allows for return to an acceptable level of function with relatively low rates of complications and reoperations in this high-risk population.
Author contributions
Sarah C. Tepper, MD – conceptualization, methodology, formal analysis, investigation, resources, writing – original draft, writing – review and editing, project administration
Linus Lee, BE - methodology, formal analysis, investigation, writing – original draft, writing – review and editing
Lucas B. Kasson, BS - formal analysis, investigation, writing – review and editing
Leyla R. Herbst, BA- formal analysis, investigation, writing – review and editing
Gayathri Vijayakumar, BS - formal analysis, investigation, writing – review and editing, visualization
Matthew W. Colman, MD - supervision, resources, writing – review and editing
Steven Gitelis, MD - supervision, resources, writing – review and editing
Alan T. Blank, MD, MS – conceptualization, methodology, supervision, resources, writing – review and editing
Author disclosures
The authors have no conflicts of interest relevant to this study.
Funding
The authors received no grant support or funding for the described work. The authors do not have any proprietary interests in the materials described in the article.