INTRODUCTION
Physiotherapists should have an overall goal of implementing evidence-based practice.1 In the field of rehabilitation after total or hemi elbow arthroplasty (TEA/HEA) physiotherapists have an important role.2 Rehabilitation can be defined as “a multimodal, person-centered, collaborative process including interventions targeting a person’s capacity and/or contextual factors related to performance with the goal of optimizing the functioning of persons with health conditions currently experiencing disability or likely to experience disability, or persons with disability”.3
In general, rehabilitation is recommended related to total joint replacement (TJR) procedures.4 Early initiation of physical therapy has demonstrated impact on functional outcomes, costs, length of stay and adverse events in the inpatient setting when compared with standard care.5 Most studies detected are on the joint sites hip and knee, and comparison of different rehabilitation protocols or regimes for other sites are hampered by few available studies and heterogeneous interventions.6–8
The elbow joint is a complex joint and has a significant importance in terms of the functionality of the upper limb.9,10 This joint has a specific role in linking two body segments, as well as in orienting the hand during everyday activities, and when impaired in function it leads to severe disability for the person affected.10
Indications for TEA/HEA can be severe inflammatory arthritis, osteoarthritis, and acute fractures.2,11,12 Pain and degree of joint destructions are the main indicators for TEA/HEA and when adequate pharmacological, and non-pharmacological treatment does not provide satisfactory symptom relief, surgery is considered the most appropriate treatment option.2,11,13
TEA/HEA are relatively uncommon orthopedic procedures.12 Results from six national registries from Australia, the Netherlands, New Zealand, Norway, the United Kingdom and Sweden, show that the number of TEAs placed annually is considerably less than that of total hip or total knee arthroplasties (THA, TKA).12 In the United Kingdom the incidence of TEA was 612 in 2017 compared to 91,698 for THA and 102,177 for TKA.12 Surgical methods and types of prostheses have been through several changes since the first surgery of TEA/HEA was performed, but the limited number of patients reported and lack of standardized assessments make it difficult to compare results.13 Even though elbow arthroplasty continues to experience substantial improvements, the complication rate also remains higher than other arthroplasties. The most common complications of elbow arthroplasty include infection, loosening, wear, triceps weakness and ulnar neuropathy.14 Further, knowledge on optimal rehabilitation after TEA/HEA is scarce.
Physiotherapists are involved in both pre- and postoperative treatment of people who undergo TEA/HEA. A central aim of the rehabilitation is to optimize recovery regarding elbow motion, often estimated as range of motion (ROM), and the ability to perform activities of daily living.2,15 To optimize rehabilitation, the importance of an individualized rehabilitation program and the precautions and functional restrictions should be clear to the patient.2 But with a lack of research-based knowledge, recommendations are mainly experience-based.15 There is a need for a more research-based approach to optimize rehabilitation and improve existing practice in this patient group. It is important to conduct a systematic search on studies regarding rehabilitation after TEA/HEA and detect knowledge gaps to help prioritize the most important future research projects.
The aim of this article is to summarize existing knowledge about the effects of systematic rehabilitation versus standard care after TEA/HEA.
METHODS
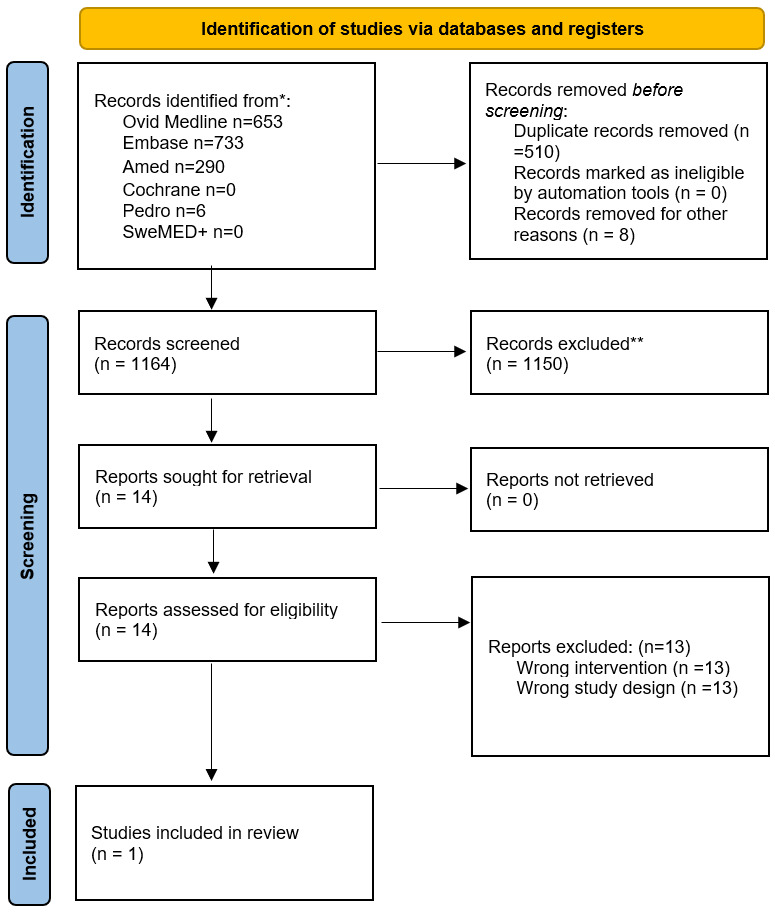
The protocol of the present systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42021282242), and is conducted in accordance with “The Preferred Reporting Items for Systematic Review and Meta-Analysis” (PRISMA) (Table S4).16 Electronic, systematic searches for relevant publications, according to the PICOS form, were conducted in November 2020 and in April/Mai 2022.
P: Patients in the postoperative phase after total- or hemi elbow arthroplasty, age >18 years. I: systematic rehabilitation / training / physiotherapy. C: regular postoperative follow-up / checks O: primary outcomes: pain, physical function. Other outcomes: Work status, complications (such as infections), quality of life. S: study design was RCTs, non-randomised controlled trials, registry studies, observational studies.
Health science librarians with expertise in systematic literature searches created the specific search strategy, and “Medical Subject Headings” (MeSH) were used to find suitable terms in addition to selected keywords in the searches. The searches were limited to publications written in English, Norwegian, Swedish and Danish. The following databases were searched to find relevant studies: Ovid MEDLINE ®, SweMED+, Cochrane, Embase, AMED and PEDro. Search histories are documented in S1.
Inclusion criteria:
-
RCTs, non-randomised controlled trials, registry studies, observational studies (retrospective studies or prospective studies)
-
age> 18 years
-
surgery with a total- or hemi elbow arthroplasty
-
description of rehabilitation / training / postoperative follow-up/physiotherapy.
-
Outcomes: Pain, physical function, work status, complications, and quality of life
Exclusion criteria:
-
published before year 2000
-
Studies on animals and cadavers
-
Case reports, case series and abstracts
One reviewer (KH) first reviewed the results from the search to delete duplicates. Furthermore, three reviewers evaluated all titles and abstracts individually, and further evaluated the articles that were selected in full text (KH, IS and SMUS).
The Newcastle-Ottawa scale for cohort studies was used for the quality assessment of included studies.17 One reviewer assessed the quality of the included study (GS), and the assessment were discussed with the other authors of the review. One reviewer (GS) extracted data from included studies, and the other authors checked the data against the full texts. For each outcome, we extracted data on all measures and all time-points. We extracted information on country in which the study was conducted, aims of the study, methods, participant characteristics, interventions, and outcomes.
For continuous outcomes, we used standardized mean differences (Cohen’s d), and for dichotomous outcomes we used risk ratios and number needed to treat to present results. If the populations, interventions, and outcomes were sufficiently similar, we planned to perform random-effects meta-analyses using Review Manager (REF). For studies with only one group, we planned to use the R package (metafor) and perform meta-analyses of proportions. We planned to construct forest plots to display results and funnel plots for exploring heterogeneity if there were results for more than ten studies. Planned subgroups analyses were total versus hemi elbow arthroplasty. If standardized mean differences or risk ratios were not reported, we attempted to convert the reported data to these measures. If this was not possible, we planned to contact the authors to obtain the data. After the protocol was published, we decided to use the Grading of Recommendations Assessment, Development and Evaluation (short GRADE) framework to assess certainty (or confidence) in the body of evidence for an outcome.18
RESULTS
A Flowchart of the inclusion process from searches in Ovid MEDLINE ®, SweMED+, Cochrane, Embase, AMED and PEDro are presented in Figure 1.
We included one study by Prki et al.19 Details of the study are presented in Table 1, and rating of the study are presented in S3. An overview of the excluded full text studies is presented in Table S2.
Prki et al19 implemented ‘functional discharge criteria’ for TEA patients. These criteria were defined as adequate mobility to resume the activities of daily living, sufficient pain control for physiotherapy exercises and a wound that addressed no further specialized care. Three cohorts were made; first the index cohort (n = 70), which consisted of all patients that received an arthroplasty before January 1st, 2016, when the institutional policy to omit casting post-operatively was introduced. Second, a cohort of patients without functional discharge criteria (n = 31) was labeled as ‘empirical discharge’. Third, a cohort with functional discharge criteria (n =25) was defined with all patients who received a primary TEA since August 2017.
Results for the main outcomes (pain, physical function): There were no results for pain or physical function.
Results for other outcomes (work status, complications (such as infections), quality of life.): There were no results for work status or quality of life.
The non-casting cohort had a shorter mean length of stay (5.4 days, SD =2.0) than the index cohort (6.2 days, SD = 3.4). A Mann-Whitney U test was statistically significant (p<0.001). Because Prki et al19 reported non-normal distributions, we have not estimated Cohen’s d.
The cohort with functional discharge criteria had a shorter mean length of hospital stay (3.8 days) than the cohort without functional discharge (5.4 days). The Mann-Whitney U test was statistically significant (p<0.001). Because Prki et al19 reported non-normal distribution, we have not estimated Cohen’s d.
Because we only included one study, we could not perform meta-analyses.
DISCUSSION
This review aimed to summarize existing knowledge about the effects of systematic rehabilitation on pain, physical function, work status, complications, and quality of life versus standard care after TEA/HEA. However, after performing the literature searches, we found no articles addressing this topic. One study was included, and the aim of this study was to look at the safety and length of stay after omission of casting, start of early mobilization and implementation of functional discharge criteria after TEA. No studies addressing HEA was included.
The study included in this systematic review addressed the use of cast and splint.19 In 2020, the book “Elbow Arthroplasty”20 were published with one of the chapters addressing post-operative management and one of the recommendations is to place the arm in a splint.2 This recommendation is in contrast to the findings in the article by Prki et al19 who report that omitting a post-operative cast in combination with functional discharge criteria led to shorter length of stay, without higher complications rates. However, although this procedure seems to be safe, and challenges some of the existing recommendations, we must take into consideration that only 125 patients were included in this study. Results of the article of Prki et al19 support that physiotherapists and surgeons should look into their recommendations for restrictions and rehabilitation after TEA. In 2006, Szekeres et al21 stated that there were no scientific papers looking at benefits of physiotherapy after TEA/HEA, but the authors believed that physiotherapy can provide benefit for these patients.21 Although this was communicated in 2006, there is little new research in this filed. Postoperative management are described in several studies,22–27 but in many cases the recommendations appear to be based on the surgeon’s recommendation and not scientific results. Recommendations for rehabilitation after TEA/HEA is largely focusing on post-operative restrictions, and further active and passive movements with the aim of increasing range of motion (ROM).2 Barlow et al28 studied the activity level of the patients after TEA and their compliance to postoperative restrictions. The results showed that only 64% of the patients accurately remembered and were compliant with their postoperative restrictions. The authors state that it is unclear whether these restrictions will provide increased longevity of the implants, but three of four surgeons counselled the patients not to lift anything weighing over 10 lb or to repetitively lift more than 2 to 3 lb.28 The fourth surgeon in this study recommended the patients to limit the total cumulative stress without specific restrictions. The authors did not report whether there were differences in activity level between the patients receiving specific restrictions and those who did not.28 It would be of interest to get more knowledge about differences in complication rate between patients receiving different recommendations from the surgeon, and further, which recommendations for rehabilitation will lead to best results for the patients.
As mentioned, we could not find any studies supporting recommendations for postoperative exercise after TEA/HEA, which is in contrast to for example other joint sites such as knee arthroplasty.29–32 Pozzi et al31 conclude in their systematic review regarding physical exercise after TKA that optimal outpatient physiotherapy protocols should include: strengthening and intensive functional exercises given through land-based or aquatic programs, the intensity of which is increased based on patient progress. Another systematic review and meta-analysis by Chen et al29 summarized the effects of progressive resistance training (PRT) for early postoperative fast-track total hip or knee arthroplasty. They concluded that PRT is one of the options for rapid rehabilitation after joint replacement.29 A systematic review addressing effectiveness of physiotherapy exercise following TKA included 18 RCTs and concluded that interventions including physiotherapy and exercise after TKA showed short-term improvements in physical function.32 Another study aimed to evaluate the effectiveness of formal physical therapy following total shoulder arthroplasty (TSA), and included one RCT in their systematic review.33 Results from this study showed that immediate provision of passive- and active-assisted ROM exercises provides short-term benefits in pain and function, when compared to a delayed approach.33 Edwards et al33 conclude in their review that there is an urgent need for high-quality, adequately powered RCTs to determine the effectiveness of rehabilitation programs following TSA, and that the volume of RCTs evaluating rehabilitation interventions following THA and total TKA is a stark contrast.32,34,35 Results from our systematic review show an even greater contrast because we found no RCTs addressing the topic rehabilitation after TEA/HEA.
The low incidence of TEA/HEA can explain some of the reason why there are less RCTs addressing rehabilitation after TEA/HEA compared to other joint sites, because it is difficult to have enough power in a study without large cohorts of patients.12 However, could results from studies regarding exercise after TKA been taken more into the discussions regarding recommendations to rehabilitation after TEA/HEA? Both of these joints are classed as hinge-type synovial joints,36 and we can ask whether the recommendation on exercise after TKA can also apply to patients who have undergone surgery for TEA/HEA. One obvious counterargument is of course the different requirements in terms of load, type of weight-bearing joints, weight arm and so on, but while restrictions after TKA are short-term, the restrictions after TEA/HEA are permanent. Because no studies have looked at rehabilitation or exercise after TEA/HEA we cannot know if these permanent restrictions are needed, or whether a structured rehabilitation program will improve complications rate and function. Complications such as loosening of the prothesis and infections are outcomes often reported after TEA/HEA.14,37,38 A question to be raised is whether these complications are related to the rehabilitation after surgery, the implant, or the surgery procedure. Perhaps a more systematic and knowledge-based rehabilitation strategy can reduce such complications, and in addition improve physical function, activities of daily living and quality of life. According to results from this study, based on research as of today, there are yet no answers to these questions.
Limitations of the review process could be the lack of automation tools used, and the possibility that we may have overlooked relevant articles. However, three persons screened the articles and were included in the selection process which reduces the risk that relevant articles have not been included.
Conclusion
No one has studied the effects of rehabilitation components or programs after TEA/HEA. The effects of such rehabilitation are unknown. Even though this is a small patient group worldwide, it is important to focus on the lack of evidence in this field, and plan for more studies to come.
Acknowledgements
We would like to thank Rikke Helene Moe for her assistance in finding current literature regarding research on rehabilitation and hip and knee arthroplasty.
Authors’ contribution
The Vancouver convention was followed. KH, IS and SMUS researched literature and conceived the study. KH (introduction and discussion) and GS (methods and results) wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Conflicting interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.