1. INTRODUCTION
Non-unions are one of the major challenges that orthopaedic surgeons must face. It is estimated that 5-10% of fracture healings undergoing surgery may be burdened by this fearful complication.1 The possible causes are numerous: inadequate osteosynthesis, incorrect pre-operative planning, excessive stripping of the periosteum, incorrect reduction of fracture fragments, but also advanced age of the patient, comorbidities, abnormalities in the peripheral microcirculation. To date, many techniques have been proposed to overcome this complication ranging from osteosynthesis revision to very complex techniques that require additional skills, such as the ability to perform a microsurgical vascular anastomosis. In particular, bone flaps are currently regarded as the treatments of choice, as they allow the bone gap to be filled with vital and vascularized bone, favouring regeneration with much higher success rates compared to other techniques that involve the use of cadaveric bone grafts or non-vascularized auto-transplants. Many bone flaps have been described, like as the vascularized fibular graft or the medial femoral condyle flap, among the best known and most used. The aim is to better adapt the flap to the geometry of the receiving bone, to the length of the bone gap, achieving increasingly less invasiveness on the donor site.
Researchers have long wondered whether it is essential to perform both arterial and venous anastomoses in bone-only flaps. It is known that the venous anastomosis, 2 veins and 1 artery, is mandatory in flaps involving soft tissues, as venous congestion can cause flap failure even several days after surgery. In the case of bone flaps, the venous anastomosis may be redundant. The reason is explained by Tanaka et al.2: the experimental study on the rat has demonstrated that the bone is able to autonomously guarantee venous drainage thanks to the cancellous tissue structure and the bone marrow, but only in case of optimal reduction and absolute stability between the fracture fragments.
Recently, Guzzini et al.,3 in a clinical study confirmed that the bone flap can survive even without venous anastomosis, guaranteeing results comparable to those in which the anastomoses were performed.. If these results are confirmed, that will reduce surgical times, granting less stress for the surgeon and lower infectious risks.
However, currently the literature is unable to guarantee certain answers on the topic because there are few systematic reviews, and to our knowledge, no meta-analysis has been published that confirms the superiority of one technique over the other.
The aim of our systematic review and meta-analysis is to report the overall failure rate of vascularized bone graft and try to answer the following question: is it necessary to perform venous anastomosis in the bone-only graft to ensure optimal survival rate?
2. MATERIALS AND METHODS
We performed this systematic review and meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.4 This systematic review is registered in PROSPERO 2025 CRD420251078628, available from: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251078628
2.1. Search strategy
PubMed, Embase, and the Cochrane Library were systematically searched in January 2025 regarding the role of the venous micro-anastomosis in the drainage of blood after microsurgical bone graft. Data relating to the studies that reported results about bone graft performed with microsurgical anastomosis of vein and artery and studies that reported the results of bone graft with only arterial anastomosis were compared. The aim was to understand if the venous anastomosis could influence the survival rate.
The search strategies are reported: (venous drainage) OR (venous return)) OR (venous anastomosis) AND (nonunion)) OR (pseudoarthrosis)) AND (microsurgical cortico periosteal bone flap)) OR (free bone transfer)) OR (microsurgical bone transfer) venous OR drainage OR OR OR venous OR return OR OR OR venous OR anastomosis OR AND OR nonunion OR OR OR pseudoarthrosis OR AND OR microsurgical OR cortico OR periosteal OR bone OR flap OR OR OR free OR bone OR transfer OR OR OR microsurgical OR bone OR transfer
(arterial anastomosis) NOT (venous anastomosis) AND (nonunion) OR (pseudoarthrosis) AND (microsurgical cortico periosteal bone flap) OR (free bone transfer) OR (microsurgical bone transfer)
Additional studies were eventually identified from the references of the retrieved papers.
2.2. Eligibility criteria
The retrieved studies were included in the meta-analysis if they were about microsurgical bone graft and reported which type of microsurgical anastomosis were performed (arteriosus and venous anastomosis or artery only) to treat bone loss following infection (resolved) or for aseptic pseudoarthrosis of the upper or lower limbs in adulthood (>15 years) and were written in English and available in full-text.
Case reports, reviews and studies only reporting microsurgical anastomosis without clear technical details were excluded from the review.
2.3. Data extraction
Two reviewers performed the data extraction independently. In case of disagreement, the first author sought to resolve the divergences.
Data extracted from the eligible studies included: author names, year of publication, sample size, type of bone graft used, site of bone loss, mean age, mean follow-up, number of failures, complications, complications of the donor site, size of bone loss, percentage of bone healing at 6 months post-op., resolved bone infection or not.
2.4. Quality evaluation
Two reviewers performed the quality evaluation of the studies independently. In case of disagreement, the first author sought to resolve the disagreements. To assess the potential risk of bias and the applicability of the evidence founded in the primary studies to the review, the Newcastle-Ottawa Scale (NOS) was adopted.5
2.5. Statistical analysis
The statistical analysis of this meta-analysis was carried out using the software ‘R’ version 4.3.1 (R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/) and the meta package.6
A random-effects model was used to perform the meta-analysis, because of the sparse nature of data and because we anticipated considerable between-study heterogeneity.
The meta-analytical methodology used was:
-
The Inverse Variance method for pooling data with arcsin transformation. This method allow to evaluate the individual study weights, even in a meta-analysis with very different sample sizes, avoiding problems with the back-transformation of the Freeman-Tukey transformation.7
-
Hartung-Knapp adjustment for random effects model.8 Several studies9,10 showed that these adjustments can reduce the chance of false positives, especially when the number of studies is small;
-
Clopper-Pearson confidence interval for individual studies11;
-
Continuity correction of 0.5 in studies with zero cell frequencies.12
The overall Effect Size of this meta-analysis are reported as proportion of failed graft (back-transformed value from arcsin transformation) and 95% confidence intervals (CIs). The proper interpretation of the back-transformed value is that it reflects the median failure risk.13
The heterogeneity was evaluated using Higgins and Thompson’s I2 statistics14 and the Restricted maximum-likelihood estimator for τ2.15 The Q-profile method was used for the confidence interval of τ2 and τ.16 Prediction intervals based on t-distribution were furthermore provided to better clarify the meaning of the heterogeneity measure reported.17
The potential sources of heterogeneity were investigated as follows:
-
Checking for outliers and influential cases by performing an influence diagnostic.18 Studentized residuals and Cook’s distances are used to examine whether studies may be outliers and/or influential in the context of the model.18 Studies with a studentized residual larger than the th percentile of a standard normal distribution are considered potential outliers (i.e., using a Bonferroni correction with two-sided for studies included in the meta-analysis). Studies with a Cook’s distance larger than the median plus six times the interquartile range of the Cook’s distances are considered to be influential. A Baujat plot was used to report the influence diagnostic.13 After we identified the influential studies, we performed and reported the results of a sensitivity analysis in which these studies are excluded.
-
Performing a sub-group analysis based on the presence of venous anastomosis (VA) during the surgical procedure, in an attempt to reduce the potential cause of heterogeneity and investigate the effect of VA on the graft survival.
-
Publication bias was investigated using Funnel Plots. The rank correlation test19 and the regression test,20 using the standard error of the observed outcomes as predictor, are used to check for funnel plot asymmetry.
3. RESULTS
3.1. Search and selection process
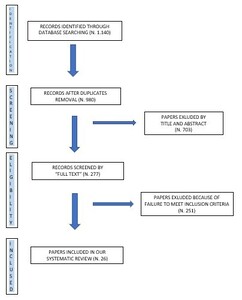
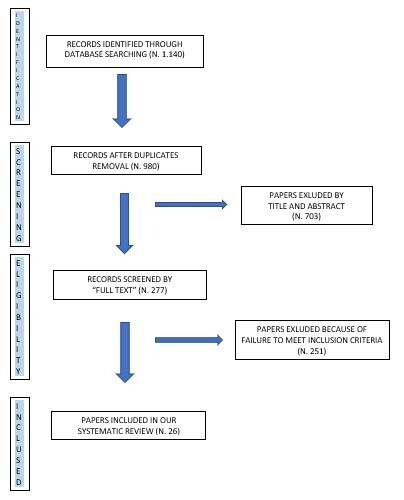
The literature search yielded 1.140 papers, from which 863 were excluded because they were duplicates or for other reasons (other languages, titles and abstracts did not match the inclusion criteria, etc.). At the end of the screening process, the full text of 277 articles was assessed for eligibility. Finally, 26 papers were included in the systematic review and meta-analysis, according to the inclusion and exclusion criteria. (Figure 1)
3.2. Included studies characteristics
The characteristics of the included studies were reported in Suppl.1. All papers were retrospective studies published from 2000 to 2023. The studies reported outcomes for fibular flaps,21–28 for free iliac crest flap24,28–30 and for medial femoral condyle in the remaining papers.2,31–43 The bone sites affected by nonunion were scaphoids and other carpal or tarsal bones and long bones of the upper and lower limbs. The sample sizes were variable in the included studies, varying from 3 to 107 cases. 6 papers reported results about cases treated with bone graft performed without venous microsurgical anastomosis (total number of cases: 155).2,36,37,39,42 The follow-up in the studies was variable, spanning from 4.4 months to 70 months. The quality analyses of the included studies reporting the Newcastle–Ottawa score are reported in Supplementary Material 1.
3.3. Meta-analysis
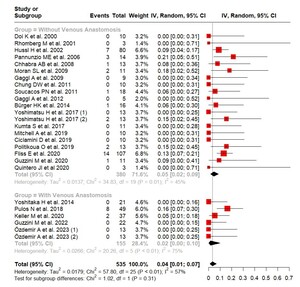
This meta-analysis included 26 studies,3,21–43 with a total of 535 observations and 44 events (vascularised graft failure). With the random effect model used for this analysis the pooled failure rate was 0.0351 (3.51%) with a 95% CI ranging from 0.0131 to 0.0673. The prediction interval ranged from 0 to 0.2093.
A forest plot showing the observed outcomes and the estimate based on the random-effects model is shown in Figure 2.
3.4. Study heterogeneity and sensitivity analysis
According to the Q – test, there was a significant amount of heterogeneity in the true outcomes (Q value of (d.f. 25) = 57.80, p < 0.01).
The between – study heterogeneity variance was estimated at τ2 = 0.0179 (95% CI: 0.0043; 0.0446), with a I2 value of 56.7% (95% CI: 33.0%; 72.1%). The analysis indicated the presence of a moderate heterogeneity.
Three studies23,26,42 had relatively large weights compared to the rest of the studies (i.e., “weight” ≥3/k, so a weight at least 3 times as large as having equal weights across studies). An examination of the studentized residuals revealed that none of the studies had a value larger than ±3.1019 and hence there was no indication of outliers in the context of this model.
According to Cook’s distances, these three studies23,26,42 could be considered to be overly influential. The Baujat plot realised for the metanalysis clearly showed this influential effect and was presented in Figure 3.
Consequently, a sensitivity analysis was made by excluding the three influential studies and obtaining a reduction in failure risk (Effect Size 0.0219 (2.19%), 95% CI: 0.0060; 0.0474) and a significantly decreased heterogeneity (τ2 = 0.0103 (95%CI: 0; 0.0338), I2 = 36.8%, Q(d.f. 22) = 34.82, p = 0.04).
3.5. Subgroup analysis
In the attempt to answer the second question of this review, if performing venous anastomosis is necessary in the bone-only graft to ensure optimal survival rate, we conducted a subgroup analysis of the papers in which venous anastomosis was made during bone grafting.
The group of papers in which the venous anastomosis was not carried out included 20 articles; the pooled failure rate was 4.54% (effect size 0.0454, 95%CI: 0.0168; 0.0870); τ2 = 0.0137; I2 = 45.4%; Q (d.f. 19) = 34.83; p = 0.01.
The group of papers in which the venous anastomosis was performed included 6 articles; the pooled failure rate was 1.63% (effect size 0.0163, 95%CI: 0; 0.1007); τ2 = 0.0266; I2 = 75.3%; Q (d.f. 5) = 34.83; p < 0.01.
The test for subgroup differences, however, did not reach the statistical significance (p = 0.3133)
The forest plot with the subgroup analysis was reported in figure 4.
3.6. Publication bias
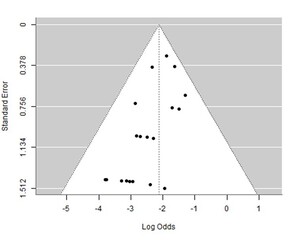
A funnel plot of the estimates is shown in Figure 5. The regression test indicated funnel plot asymmetry but not the rank correlation test
4. DISCUSSION
Bony defects can be secondary to many clinical conditions: trauma, infections, tumors, and require complex approaches to minimize the risk of patient morbidity and restore good function. The first known bone transplant took place in the seventeenth century.44 Since then, vascularized bone transplants have always been preferred over non-vascularized ones, for their best abilities to osteointegrate and remodelate thanks to the blood supply. It is in fact known that non-vascularized bone grafts have the only effect of being osteoinductive, stimulating the formation of new bone starting only from the neighboring vital one and therefore are not particularly suitable in cases of atrophic or septic environments.
However, vascularized bone transplants require particular surgical skills, primarily the microsurgical ones to perform the vascular anastomoses.
It is known that the bone tissue is intrinsically able to drain the venous blood because of its peculiar anatomical characteristics: it can occur through the medullary canal in the presence of absolute stability. The aim of our meta-analysis is to clarify whether or not it is really necessary to perform venous anastomosis in bone transplants. In 2001, Kamei et al. reported the case of a 26-year-old patient who underwent a free fibula bone transplant due to severe loss of substance in the contralateral tibia and adjacent tissues. The development of a complication made it possible to appreciate how the bone can self-manage venous outflow. In fact, the flap underwent two episodes of venous re-thrombosis, but it did not fail thanks to the venous drainage obtained through the bone marrow.45
On the other hand, the vascular potential that characterizes the bone tissue from others, is confirmed also by the technique of arterialized venous flaps (AVFs). These are tissue flaps harvested without conventional vascular pedicles. In particular, it is achieved by anastomosis of a recipient artery to the venous plexus within the flap. The exact mechanism that leads to the survival of the bone graft is still unclear, but it confirms the hypothesis that the bone venous system works according to mechanisms that can justify the modification of the normal microsurgical techniques applied to these flaps.46
The findings of our review are not definitive due to the inherent limitations of meta-analyses conducted with observational studies. Consequently, we urge caution in asserting that venous anastomosis is superfluous, as it appears to provide a protective effect against failure, despite not reaching statistical significance. To our knowledge, Guzzini et al. are the authors who have performed a prospective study aimed at demonstrating the superfluous nature of venous anastomosis, and their data support this hypothesis.3
On the other hand, it is known that slow venous drainage can also cause ischemic suffering of the bone if alternative drainage systems, e.g. bone marrow, are not perfectly functioning. In particular, failure increases in case of non-absolute stability between bone graft and recipient bone. Therefore, although it is advisable to always perform a stable and valid osteosynthesis, also performing the venous anastomosis offers greater guarantees of success to the surgeon.
Already in 1993, in an experimental study, Janowski et al. tried to demonstrate the effects of venous occlusion in a bone transplant and studied the differences, including histological ones, compared to the traditional technique. The authors demonstrated that the vascularized graft healed earlier than the corresponding vascularized one with venous occlusion. The latter healed but with a variable amount of bone necrosis, followed by resorption, which delayed its integration.47
Our meta-analysis presents some limitations. All the articles included are retrospective and observational studies. No RCTs on the topic are currently present in literature, to our knowledge.
Synthesising observational studies (OSs) is at high risk for within - studies and cross - studies biases and burdened with the presence of increased heterogeneity, for both methodological and clinical reasons.48
Despite these issues, results from OSs present however some advantages. For some clinical questions, for example, RCTs are not available or not feasible, making OSs the only available source of evidence. In addition, being OSs often conducted in real-life scenarios, it makes the results more generalisable than RCTs.
Another limitation is due to the different nature of the surgical procedures performed in the included studies, that can increase the across-studies biases.
Our meta-analysis, however, has some advantages, as well: the high number of cases studied and the diversification of the skeletal segments treated.
5. CONCLUSION
Bone transplants are a vital therapeutic approach for addressing bone defects, consistently delivering excellent results. While venous anastomosis is not strictly necessary to prevent transplant failure, it may offer a protective benefit. Further studies with higher levels of evidence are needed to confirm this.
Authors’ contributions
MS and FS: Conceptualization and Methodology; MS and VC: Data curation, Writing- Original draft preparation; GB and SS: Visualization, Investigation; GM and MM: Validation and Supervision; AB and DML: Writing- Reviewing and Editing.
Consent for publication
Not applicable
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
Nothing to declare
Funding
Not applicable
Acknowledgements
Not applicable